WNS recently briefed me on its Digital Policy Administrator (DPA) solution/platform, a patent for which is pending and is not yet publicly available. The DPA is positioned as a utility-style third-party administration (TPA) platform for the life and annuities (L&A) sector, built to reduce the burden of legacy technology debt and enable faster rollout of new products.
Market Challenges in L&A
Carriers in the L&A sector face persistent structural challenges. Productivity gains have lagged other industries, even as cost pressures mount. Carriers continue to operate on aging legacy technology platforms, increasing complexity and slow responsiveness. Product innovation cycles are lengthening, just as market volatility and interest rates drive greater demand for flexible annuity products.
Outsourcing is widely used, but it has not resolved these challenges. Four of the top five L&A carriers already outsource parts of their administration. Still, most TPAs remain anchored to labor-intensive delivery models with limited automation. As a result, carriers are unable to fully escape the inflexibility and inefficiency challenges they face.
WNS’ Position in Insurance
Insurance contributes roughly a quarter of WNS’ total revenue, highlighting the importance of this vertical to its overall strategy. It supports ~70 active insurance engagements, employing ~18k insurance specialists. Within this workforce are ~650 actuarial professionals, ~500 data and analytics experts, and ~5k customer experience specialists. The practice also leverages ~50 digital solutions and accelerators to support engagements across all insurance engagements.
Recent acquisitions extend WNS’ digital toolset. Vuram, acquired in 2022, brought automation and BPM capabilities, while Kipi.ai, acquired in 2025, enhanced GenAI development. Together, these acquisitions create a transformation-led approach that is now in ~90% of WNS’ insurance engagements.
Addressing Core L&A Challenges
WNS’ Digital Policy Administrator is designed to address two core barriers for L&A carriers. First is legacy debt: policy administration, billing, claims, and reinsurance are frequently handled on outdated systems that are costly to maintain and difficult to modernize. Second is the challenge of slow product rollout cycles, which prevents insurers from capturing emerging demands in a timely fashion.
WNS positions the DPA as an integrated solution combined with core systems, with proprietary platforms, automation, and global delivery in mind. The objective is to offer insurers an option beyond piecemeal outsourcing, a packaged TPA model focused on measurable efficiency and configurability with speed.
A Utility Model for Policy Administration
The DPA is designed as a utility service rather than as a customized, one-off deployment. Its design principles are straightforward but ambitious. The delivery model follows an automation-first philosophy. In practice, this means processes are automated wherever possible before being offshored; only the most complex elements are retained onshore. The principle is not just to focus on cost optimization but ensuring standardization and consistency across servicing operations.
WNS chose to partner for the policy core rather than build its own. The rationale was speed and flexibility; deploying a proven core accelerates adoption while avoiding heavy in-house development cycles. The platform is cloud-deployed, API-enabled, and designed to support per-policy pricing, aligning costs with actual business volumes.
This avoids lock-in by incorporating open-source components where feasible. Change is driven by configuration, not code rewrites, maximizing reusability and ensuring the system remains upgradable. These design elements support a packaged TPA model that is scalable and adaptable to client needs.
Architecture: Automation-First Design
At the center of DPA is Verisk FAST, the chosen core policy platform. FAST provides new business, policy administration, billing, claims and reinsurance in a microservices and API-based architecture. It minimizes reliance on middleware and reduces the need for patchwork integrations.
Surrounding the core is a set of platforms and frameworks:
- Skense, WNS’ proprietary intelligent document platform for ingestion, triaging, and indexing
- Ushur, supporting voice-to-text, agent assist, and automated outbound correspondence
- Genesys, providing omnichannel routing, IVR, and speech analytics
- Framework integrations, connecting to general ledger systems, policy and agent data, reinsurance, illustrations, and e-applications.
Together, this ecosystem enables straight-through-processing and reduces manual interventions. Automation is designed into the workflow from the start rather than being layered in afterward.
Global Delivery Model
The DPA is powered by WNS’ global delivery model. Work is distributed by geography and complexity. Policy servicing, billing, and collections are managed through back-office teams in India. Voice operations are delivered from South Africa and the Philippines. For complex or high-touch needs such as complaint management, WNS provides onshore delivery to ensure responsiveness and quality.
Supporting layers include IT service desk, infrastructure and security, HR, F&A, and governance/compliance functions.
Early MVP Flows
One example of early product flow is beneficiary change processing, where Skense ingests change request documents and FAST executes the policy updates with no manual interventions.
Additional flows are being added, including surrenders, licensing, and commission management, demonstrating the platform’s ability to move beyond simple transactions.
Target clients are threefold: existing WNS insurance BPO clients looking to modernize, new clients seeking an integrated TPA platform, and current FAST users exploring an overlay model with WNS services.
WNS’ Outcomes with DPA
WNS claims several measurable outcomes from the DPA platform. New product setup can be completed in six to eight weeks, supported by API integrations. The SaaS core is configuration-driven, enabling upgrades without code rewrites. Automation and GenAI augmentation are expected to reduce error rates and operational costs. Pricing is aligned per policy, with fixed implementation costs.
Roadmap for Expansion
AI capabilities are planned to expand into predictive claim prevention, underwriting automation, and advanced pricing models. These additions are positioned to move the platform transactional efficiency toward decision support. The framework is designed for geographic adaptability. WNS has developed an ecosystem framework to allow substitution of core systems to meet geo-specific product requirements, enabling flexibility for clients to operate with technology tailored to their market needs. WNS is currently executing this in the U.K. and Australian markets. It also plans to extend framework services with additional partner integrations and digital servicing capabilities, reflecting insurer demand for configurable ecosystems rather than rigid, closed deployments.
Outlook
The DPA signals WNS’ bid to reposition L&A administration as a standardized utility rather than a labor-led outsourcing model. Anchored on Verisk FAST and supported by proprietary IP (e.g., Skense), the platform reflects an automation-first philosophy designed to scale beyond piecemeal modernization efforts.
While many TPAs and policy administration systems are already moving toward cloud-based, API-enabled, and automation-augmented models, most progress has been incremental and concentrated on standard transactions. Complex flow often remains heavily manual, and pricing still leans towards fixed contracts rather than usage-based structures. Few offerings in the market have demonstrated a fully standardized utility-style model that combines automation across simple and complex flows with per-policy economics and global delivery at scale.
The real test is whether carriers will entrust a third-party utility with functions historically viewed as too core to externalize. Early MVP flows (beneficiary changes, licensing, commissions) are a proving ground, but large-scale adoption will hinge on demonstrating resilience, compliance, and cost predictability under production conditions.
If WNS succeeds with this nascent offering, the DPA could reset expectations for L&A policy administration by introducing per-policy economics, faster product adaptability, and a scalable alternative to fragmented outsourcing. If execution falters, it risks becoming another example of a TPA promising modernization without delivering differentiation. The upcoming 12 to 24 months after market introduction will determine which outcome prevails.
]]>
EXL recently briefed me on how it is leveraging agentic AI in the insurance industry, a sector that is at a turning point in its AI journey. Early experiments with large, general-purpose models have proven what’s possible, but they’ve also revealed what does not work. Hallucinations, high costs, and generic outputs are incompatible with an industry built on precision, regulation, and trust. The next phase of AI in insurance is not about size, but about fit, embedding intelligence directly into workflows, tuned to exact personas that power the insurance value chain.
EXL is combining access to proprietary data with fine-tuned, lightweight models, moving beyond demonstrations of AI potential into real-world deployment. Its approach is rooted in a simple but core concept: building AI agents that think, behave, and make decisions like insurance professionals.
Why General Models Are Not Enough
The promise of massive LLMs like GPT-5 or Gemini is undeniable. They are powerful tools for research, writing, and general reasoning. But in insurance, the stakes are different. Claims adjudication, underwriting, and fraud detection demand more than a generalized understanding of language. They require context, accuracy, privacy, and compliance, all while operating within cost constraints.
A generic model might summarize a news article. But it cannot reliably triangulate 800 pages of medical records, calculate fair claim valuations, or spot subtle fraud indicators buried in policy notes. Bridging the gap between general potential and domain precision is where EXL is building an advantage.
Persona-Based Domain Models
Rather than chasing the biggest model, EXL is building smaller, purpose-built models that mimic specific roles inside an insurance organization. Claims specialists, underwriters, and subrogation adjusters each have their own reasoning process, data dependencies, and decision criteria. By training lightweight models on proprietary derivatives datasets, EXL has created a portfolio of “co-workers” designed to fit seamlessly into insurance operations.
This persona-based approach is reinforced by a deliberate balance across five design factors: accuracy, hallucination control, cost efficiency, data privacy, and latency. The result is AI that not only works, but works in production environments when regulators, clients, and customers demand reliability.
Use Cases Across the Value Chain
Claims Adjudication/Medical Claims Review
- AI agents summarize months of claim history into clean, chronological narratives
- Adjusters can query claims directly with natural language questions, retrieving answers instantly
- Document intelligence agents process incoming files and communications, updating propensity models for fraud, recovery, or liability. In some cases, they even draft recovery letters automatically
- In workers’ compensation, disability, and liability lines, medical files average 500-800 pages
- EXL’s models tag ~40 key sections, generate structured summaries, and deliver consistent interpretations that reduce reliance on overburdened medical staff, eliminating human error.
Life Underwriting
- Finely-tuned models triangulate across medical, financial, and lifestyle data to recommend underwriting decisions
- Instead of a weekly manual review, underwriters gain structured insights in minutes.
Property Underwriting (Multimodal)
- Moving beyond text, EXL integrates images from mobile apps, drones, and satellite surveys
- AI agents review property images to surface underwriting concerns, allowing underwriters to make faster, more informed decisions.
Intellectual Property and Market Adoption
This work is not just conceptual; EXL has secured a U.S. patent for its insurance LLM, with additional patents underway for Claims Assist and other solutions. Early adopters in APAC, the U.K., and the U.S. are already deploying modules, whether for claim summarization, fraud propensity scoring, or recovery optimization
The modular design is intentional. Insurers no longer have to rip and replace existing systems. Instead, they can embed targeted AI agents where pain is the greatest, cutting review times, improving decision quality, and reducing costs step by step.
Why it Matters
For insurers, the benefits are clear:
- Efficiency: reducing adjuster review times from 20-25 minutes to seconds
- Consistency: minimizing variation inherent in human-only decision making
- Cost savings: leveraging lightweight models that are cheaper to run than mega-LLMs
- Scalability: applying persona-based designs across lines of business and geographies.
But the bigger story is cultural. Insurers are moving away from AI as an “experiment on the side” and into a future where intelligence is embedded directly into the workflows that define their business.
The Right Model, Not the Biggest Model
The race to build trillion-parameter models makes headlines, but the more pressing question is who has the right model. EXL frames its agentic AI approach as a way of thinking differently about adoption, one that is persona-based, lightweight, and modular, rather than generic or monolithic. By training models to act like adjusters, underwriters, or surveyors, EXL is positioning itself to help insurers address pain points where efficiency and consistency matter.
From an industry perspective, this is notable. Insurers continue to test and experiment with large, general-purpose models, yielding mixed results, as they encounter challenges with accuracy, privacy, and cost. Agentic AI offers a bridge between experimentation and operational adoption. EXL’s proprietary data rights and patent-backed IP are designed to provide a durable foundation for building agentic AI capabilities tailored to the needs of insurance clients.
The approach and opportunity presented here are promising, though hurdles are to be expected along the way. Adoption has already begun in claim summarization, recovery scoring, and underwriting support, and is expected to extend further into decision-heavy functions where explainability and regulatory oversight will be critical. If agentic AI develops as EXL anticipates, it will not only improve near-term efficiency but possibly reshape how insurers structure work and allocate expertise across the value chain in the years ahead.
]]>
In a recent discussion, NelsonHall explored how WNS HealthHelp continues to modernize utilization management (UM) through scalable AI, real-time decision-making, and configurable service models.
WNS HealthHelp’s platform, Consult™, builds on its evidence-based clinical guidance and continues to achieve high ROI and provider satisfaction through automation and more collaborative provider engagement. For example, within cardiology, musculoskeletal, sleep, and surgical services, a health plan leveraging WNS HealthHelp observed a ~50% drop in denial rates while maintaining stable saving levels.
Accelerating Clinical Decision-Making Through AI
WNS HealthHelp has accelerated its investment in AI across the workflow's intake and nurse review layers. A core enhancement is integrating an AI engine that processes submitted clinical documents, matches them against guidelines, and returns decisions within minutes. This innovation removes avoidable delays and enables providers to be productive while the patient is still in the office.
Unlike traditional UM models, where nurses manually triage all submissions, WNS HealthHelp’s engine ensures that only nuanced or incomplete cases reach their Nurse Review or Specialty Provider Outreach sections. As a result, its clinicians, many of whom are active specialists, can focus on high-impact cases that require true peer-to-peer consultation.
A Modular ’Choose Your Own Path’ Model
Health plans are no longer restricted to rigid UM outsourcing arrangements. WNS HealthHelp now offers three service models:
- UM Elite – fully delegated, WNS-managed solution with end-to-end coverage including technology, expert resources, including medical directors, and clinical staff
- UM Plus – shared technology and resources that extend the payer’s internal capabilities
- UM Standard (BPM) – client-run tech stack paired with WNS clinical and operational support.
These flexible models allow payers to align UM support with their internal strategy, whether scaling fast, minimizing abrasion, or improving turnaround time.
WNS HealthHelp also offers flexible pricing models designed to accommodate different levels of engagement. Options include transaction-based pricing, shared savings agreements, and guarantee-based models tailored to performance metrics. This approach enables health plans to align financial risk with service scope and outcome goals, whether they are pursuing full delegation or targeted support. Notably, the pricing structure is particularly attractive to Medicaid plans and smaller regional payers who need high-impact solutions without taking on the cost or complexity of fully managing UM in-house.
Strengthened Partnerships, EMR Integration, and Clinical Content Expansion
WNS HealthHelp continues to expand its reach and interoperability through a strategic partner ecosystem focused on clinical optimization and provider experience. For example:
- For Humata, WNS supports EMR-integrated workflows that simplify case intake and reduce time spent on case creation
- Through its Availity partnership, WNS integrates its portal capabilities into Availity’s front-end interface, allowing providers to initiate authorizations and access clinical resources within a familiar environment
- In collaboration with Anterior, WNS enhances the clinical integrity of its AI engine, leveraging Anterior’s expertise to improve the efficiency of clinical review processes
- The partnership with InformedDNA allows WNS to rapidly scale its genetic testing programs by incorporating best-in-class clinical guidelines and certified geneticists, helping clients manage complex oncology and precision-medicine cases.
Advancing Provider Collaboration and Outcomes
Rather than relying on denials to drive savings, WNS HealthHelp focuses on changing provider behavior through clinical education and consultative engagement. The model uses matched specialists, such as cardiologists speaking with cardiologists to reach agreement on care plans, resulting in lower abrasion, fewer repeat submissions, and improved long-term outcomes.
WNS HealthHelp reports significantly higher net promoter scores than the industry average, driven by its high-touch, consultative approach, and physician-matched peer reviews.
Looking Ahead: Scaling for the Future
WNS HealthHelp is continuing to evolve its offerings with a focus on flexibility, AI integration, and reduced administrative burden for providers and payers alike.
Future roadmap priorities include expanding AI across additional intake and clinical decision layers, enhancing voice automation for call center efficiency, and introducing new analytics capabilities to track order patterns and utilization trends.
WNS is also working to commercialize its internal tools for broader market access, making it easier for payers to adopt individual components (e.g., clinical guidelines engine, nurse AI review, intake automation) as standalone services.
With growing interest from Medicaid and regional health plans, WNS HealthHelp is well-positioned for the next phase of UM transformation by combining proven savings with improved provider experience.
]]>
NelsonHall recently attended the DXC Connect Insurance Executive Forum in Charleston, South Carolina. The event highlighted DXC Technology’s investment in AI-driven solutions for the insurance industry. A key theme was DXC’s commitment to helping insurers address their ‘technology and process debt’ through community-driven collaboration, enhanced application modernization, and AI-driven operational effectiveness using its DXC Assure platform.
Community-driven collaboration
DXC, like other companies, aims to capture industry insights through advisory councils. In particular, DXC uses structured AI advisory groups to identify and prioritize insurance-specific AI solutions over generic options. Ongoing knowledge feedback loops between client engagements are then incorporated into system testing of these emerging concepts against real-world insurance industry challenges for further model refinement.
Insurers face substantial technology & process debt
A substantial amount of technology and process debt is being faced in the insurance sector, representing ~$180bn-$200bn in hidden costs tied to maintaining legacy systems. Approximately 70% of IT budgets is consumed by legacy system maintenance, and insurers struggle with complex integrations that inflate costs and prolong implementation timelines. These complexities can compound over time with temporary workarounds, further exacerbating technical debt. As a result, insurers often experience deteriorating customer experience despite significant investments.
DXC is addressing these issues through emphases on IT modernization, automation, and cloud-agnostic solutions guided by its ‘racetrack’ framework, providing insurers with targeted maturity assessments and actionable insights.
Hastening application modernization
DXC has introduced products to hasten and facilitate application modernization. These include:
- Community Accelerator – an AI-driven framework to facilitate rapid, community-wide deployment of product updates and enhancements to reduce redundant development efforts
- Conversion Accelerator – combining insurance domain expertise and AI-powered tools to streamline insurance application modernization and reduce process complexity.
Streamlining and expediting policy & claims management
Key AI-led automation initiatives include:
- Assure BPM – to enhance operational efficiency across the insurance policy life cycle with AI-driven data integration and workflow optimization. DXC platforms are integrated with ServiceNow to optimize and streamline policy management, billing, and payment processes to improve the customer experience
- Assure Claims – to accelerate claim processing and improve fraud detection. Assure Claims incorporates intelligent document processing (IDP), using GenAI to extract structured and unstructured data from multiple document formats and leveraging historical data to increase levels of fraud detection
- Assure Answers – a GenAI capability that supports use cases such as an AI-powered chat service for underwriting, policy, and product or claim documentation summaries. For example, it can expedite processing policy cancellations, achieving a targeted ~30% reduction in cycle times. This is driven by the intelligent policy cancellation workflow:
1. The policyholder initiates the process by sending an email to notify the insurer of their cancellation request
2. DXC Assure Answers automatically verifies both the email and policy information contained within the email
3. The CRM dashboard is automatically updated, classifying the policyholder’s request as a ‘cancellation’ to ensure accuracy and eliminate manual errors
4. The cancellation is then processed, and a confirmation email is sent to the customer. This automation reduces dependency on manual intervention and allows staff to redirect their efforts toward more high-value, customer-centric activities.
Summary
DXC Technology is targeting the insurance industry’s dual challenges of technology and process debt, empowering insurers to modernize legacy platforms more effectively and mitigate risk before technological and process debt reaches a critical inflection point. At the same time, the company is introducing GenAI to enhance operational efficiency and insight across underwriting through claims management.
]]>
In recent discussions with WNS, NelsonHall explored the company's advanced healthcare management solutions. WNS provides evidence-based criteria to guide providers in ordering the most appropriate tests, procedures, and treatments for their members. This approach enhances patient care delivery and outcomes while improving provider relations and reducing healthcare treatment costs.
For example, a regional health plan was experiencing high prior authorization denial rates and provider dissatisfaction. The WNS Consult™ platform led to a demonstrated net direct savings ROI of 4.9, improved provider satisfaction and overall savings, and reduced prior authorization denial rates.
WNS’ model is proactive and focuses on behavior change rather than denial of services. It involves proactive outreach to ordering providers, offering clinical education with in-house clinicians, and modifying treatment plans to suit patients’ needs while reducing denials and abrasions.
It aims to continue to reform clinical guidance and authorization in two ways: a rigorous approach to clinical guideline development, and leveraging smart technology. At the same time, WNS offers a flexible approach to which activities it performs and which are retained in-house.
A Rigorous Approach to Clinical Guideline Development
Clinical knowledge is derived collaboratively and utilizes ~600 clinicians while promoting proactive peer outreach and integration of practicing physicians. This ensures that clinical decision-making includes comprehensive medical knowledge and real-world practice, leading to the efficacy of healthcare plans.
The platform’s clinical guidelines are based on research across:
- Governmental quality and regulatory guidelines
- Specialty society guidelines
- Evidence-based literature.
The governance model uses an independent panel comprising WNS clinicians and subject matter experts who review and update guidelines quarterly across ~400 topics and seven specialties. This process ensures that the evidence-based guidelines reflect the latest medical research and regulatory standards. These guidelines are then translated into detailed business rules that guide the Consult platform’s clinical decision-making process with branching logic, if-then, and ‘re-direct’ (auto-approval) rules.
Streamlining Authorizations with the Consult Platform
The authorization process begins with an order request submitted by the ordering physician through various channels (e.g., phone, fax, web, EHR). It enters the Consult platform and into its regulatory rule engine, which deciphers the requests against business rules and clinical guidelines. If the rule criteria are not met, the request progresses through a three-tier assessment and review before a denial or authorization is granted:
- Tier 1 – Initial assessment conducted
- Tier 2 – Nurse review
- Tier 3 – Peer-to-peer review.
If an order reaches Tier 3, the peer-to-peer review determines the appropriate course of action, which can result in a major procedure change or withdrawal of the order request. At any of the tiers, notifications are sent to the ordering provider and member if authorization is granted. If a request is denied, WNS issues a denial letter and handles all administrative communications, including denial language.
The Consult platform supports EMR connectivity and API-based architecture to provide seamless integration with existing healthcare systems, facilitating real-time data exchange, and improving the responsiveness of healthcare services. The platform has achieved ~80% automation and ~70% portal adoption, demonstrating high efficiency and user engagement.
The application of predictive analytics and AI within Consult allows for more intelligent decision-making and enhances the ability to forecast patient care needs and outcomes more effectively.
Offering a Flexible Service Model
Recognizing the diverse needs of health plans, WNS offers both delegated and non-delegated models, allowing for flexible integration of their services according to the strategic goals of the health plan. These models range from handing over everything from case intake to appeal management to WNS (delegated model) to health plans opting for non-delegated models, keeping certain services in-house (such as medical necessity decision and appeal management).
Looking Ahead: Continuous Improvement and Expansion
The WNS future roadmap includes clinical and non-clinical investments. Clinical expansion includes increased coverage of genetic testing, oncology clinical pathways, and post-acute programs. The non-clinical expansion includes enhancing the platform’s capabilities to include order pattern intelligence, UMaaS, and enhanced member engagement.
WNS’ initiatives will continue to offer improvements in how healthcare services are managed and delivered, leading to better outcomes for all stakeholders.
]]>
NelsonHall recently attended the DXC Connect Insurance Executive Forum in Charleston, South Carolina, where the theme was ‘Connecting the world’s largest insurance community to solve challenges and drive value’. DXC focused on:
- Its new product strategy to meet insurers’ transformation and investment needs
- The ability to combine its SaaS solutions with BPS to offer BPaaS services
- AI-based enhancement plans.
New product strategy launch
DXC has adjusted its product strategy to enable its clients to adopt an investment strategy or strategies dependent on their level of need to transform vs. minimize new investment. The key elements are:
- Protect – aims to safeguard organizations’ present investment while improving their existing capabilities, managing systems, and refining their environment for optimal performance. This is suitable for organizations that wish to minimize their investments while modernizing their infrastructure and optimizing their running costs by moving to a consumption-based cloud model
- Extend – access to innovative solutions, leveraging APIs and AI, and ensuring a secure system of records. This is the next step to add new functionality incrementally. Here, DXC stresses the importance of an ecosystem approach, though based on the client retaining their existing core insurance platforms. This involves incorporating these platforms into a wider ecosystem with approaches such as RESTful APIs. The ecosystem then facilitates co-innovation through access to additional point solutions, adding new capability and flexibility to switch functionality in and out
- Transform – for organizations looking for a more fundamental IT modernization. This involves digitalizing with AI and cloud-enabled solutions, making new upgrades to the DXC Assure platform, and operating in a more transformative model.
DXC’s improvement and investment strategy is strongly influenced by its user groups. Over the last year, DXC has made ~466 total enhancements to its P&C solutions, and 49% of these enhancements were community-led.
P&C BPS powered by DXC’s Assure
DXC’s Assure SaaS platform enables insurers to efficiently accelerate expansion capacity to new markets/geographies, with DXC BPS personnel providing access to expertise and support options tailored to the client’s transformation journey. DXC provides support across all 50 U.S. states; it will enhance, run, and maintain platforms and currently supports ~$2.6bn of direct written premiums.
DXC supports all insurance LOBs (e.g., workers comp, flood, commercial, specialty, and personal) and notifications services clearinghouse with ~4k trading partners, 40k endpoints, and robotic enablement.
DXC provided a use case of an insurer receiving 1,000 emails with attached documents and involving manual triaging of e-mail type, classification, and data re-entry, leading to inefficiencies in processes and increased chances of human error. DXC leveraged DXC Assure Submission and applied AI and ML. 95% of submission emails were converted to actionable data within 2 hours of receipt with a ~90% accuracy rate.
AI enhancement to DXC Assure solutions
DXC is making a major push to leverage generative, predictive, and cognitive AI solutions. They have established an AI strategy which focuses on three core areas:
- Customer AI – for improved customer experience, areas of change include a hybrid call center, real-time sentiment analysis, and GenAI knowledge assistants
- Company AI – for operational efficiency, appropriate knowledge management, and improving business outcomes
- Community AI – for a collaborative approach with real-time feedback and easier use of innovation.
AI-based enhancements that will be available in Q2 2024 include:
- DXC Assure Legal – end-to-end litigation management solution leveraging AI to automate processes for guideline compliance. Allows greater visibility and control over legal spend, leading to less time reviewing invoices
- DXC Assure Claims – partnering with AWS, a new omnichannel function that enables claims professionals to initiate texts and calls from the claims system. This addition reduces the time needed to resolve claims and furnishes a thorough audit trail of the interaction
- DXC Assure Submissions – leveraging AI and ML to extract data from semi-structured and structured submission documents. The AI is taught to distinguish critical data points from unnecessary data, reducing processing time and error rates
- DXC Assure Cede – integrating GenAI capabilities to enhance data in real-time as users navigate the system. The platform examines current SOPs, manuals, and documents to offer instantaneous summaries, enhancing productivity and user experience.
Next, DXC is further extending its AI use cases to reinsurance and Australia’s workers’ comp, both areas in which the company is already active.
Conclusions
- DXC is aiming to offer smooth migration paths from on-premise legacy insurance solutions to AI-driven SaaS and BPaaS services
- It is developing ecosystems of complementary solutions that insurers can adopt on a plug-and-play basis via APIs
- While not all GenAI PoCs will be successful and become widely deployable, DXC is making a major push to incorporate generative, predictive and cognitive AI into all its insurance modules.

In 2020, the U.S. healthcare payer BPS market saw accelerated growth in the adoption and design of digital solutions across all functional areas. The acceleration is driven mainly by consumer demand for an "Amazon" experience from their health plans and providers, to know the cost of care for associated benefit plans to assist in plan selection or inform decisions about elective procedures and treatments. It is also driven by approaching federal regulation deadlines. Specifically, regulatory requirements from the Cares Act and subsequent rulings from CMS are driving further steps towards interoperability throughout 2021-2024. These requirements follow the initiatives by CMS offering price lookup tools for outpatient procedures and OOP costs for physician visits for Medicare consumers.
Regulatory deadlines drive digital adoption
By January 1, 2022, private payers and group plans must standardize data files to be made publicly available and shared through APIs. The available data will be an opportunity for insurtechs and technology vendors to develop price comparison tools further and price analyses to inform their development.
After January 1, 2023, these payers must offer online plan comparison tools for consumers to view negotiated provider rates and personalized OOP costs estimations for 500 commonly utilized services. This will require real-time underwriting and price aggregation and analysis, with the ability to segment the data by facility and provider. Then, starting on January 1, 2024, individual and group plan consumers will be able to view the estimation of the total OOP costs, including usual tests, procedures, DME, and other items associated with specific treatment plans.
Opportunities for tech vendors to provide services & digital solutions
Without significant digital transformation, meeting the interoperability and price transparency requirements poses a considerable challenge for U.S. healthcare payers. Legacy and "home-grown" systems perpetuate siloed digital solutions, unstandardized data, and difficulties in designing APIs and intake of external data. The disjointed process becomes even more complicated when payers face these challenges on a seasonal basis to perform market assessments, develop products, and price new and renewed plans.
Additionally, payers face the challenge of complying with continual changes in required API formats, currently defined by HL7's FHIR. Payers will need support in converting or implementing the standard format and subsequent testing as regulations and required formats change, such as federal exchange marketplace plans that must implement FHIR APIs with third-party apps for open data access.
Capgemini spotlight: price transparency offerings
U.S. healthcare payers can obtain digital solutions to support regulatory compliance with Capgemini's price transparency solutions. Capgemini has 15 years of experience in the Medicare Advantage space, providing enrollment and member account maintenance management services, solutions, and advisory support. The recent focus has been on designing analytic and AI-driven tools for healthcare payer and provider clients in meeting regulatory guidelines and customer-driven demands for enhanced digital experiences and upfront cost estimations.
Capgemini offers service-line driven pricing for the average cost of medical care from hospitals and healthcare providers in the consumer's area. Capgemini developed the relative pricing guidance for hospitals, with an average of 1200 parameters per hospital for ~700 hospitals, categorizing both operational and overall spend by diagnosis parameters. The hospitals were then ranked into low, medium, high. In addition to overall price analysis, Capgemini parsed hospital spend by service line to provide cost estimations by diagnosis or treatment.
Capgemini is also working with several Blues to estimate OOP cost projections viewable on the member portal. Capgemini designed a cost calculator for a medical procedure at a specific healthcare facility, including the member's expected copay/deductible. A pricing engine was then implemented into a Blue's member portal to provide hyper-personalization, utilizing both internally available eligibility data and the aggregated market data for variable cost pricing. Currently, Capgemini offers implementations of ranking engines enabled by pricing algorithms and provider registries, returning search results of the top 10 providers most relevant for a specific diagnosis or procedure and the estimated cost of copay/deductible/OOP for each provider.
Capgemini's price transparency work is also heavily focused on utilizing MLR for cost-sharing estimations, including telehealth in the cost estimations. For a U.K. health plan, Capgemini implemented a solution to perform plan comparisons against industry standards, such as a specific member with a particular set of demographics and health characteristics, to estimate the eligibility and cost-sharing – competitive pricing. The solution incorporated several analytics tools to perform analysis and reporting on historical cost-sharing.
By the end of 2021, Capgemini's digital solutions in price transparency will integrate the payers' provider search tools to rank relevant providers based on health outcome metrics. Capgemini continues working with certain Blues plans to develop a marketplace with shared data and real-time quoting for care pricing and plan comparisons, involving interoperability and price transparency initiatives to benchmark the cost of services by area and plan. Additionally, Capgemini's development is focused on creating bundled pricing for all procedures and tests associated with a long-term treatment plan, as will be required of healthcare payers by 2024.
Increased demand and opportunities for digital transformation in the near future
The challenges faced by U.S. healthcare private and group payers present opportunities for technology vendors to provide digital solutions and services for payers to meet both the regulatory requirements and consumers' digital experience expectations. Client engagement types will vary by payer size, as many large payers only require specific solution design and implementation within their existing systems, while many mid-market and regional plans will be looking for BPaaS models of engagement with technology vendors. Payers will be looking for digital solutions to provide personalized real-time quotes for procedures and later for bundled pricing by the treatment plan and expanded data sharing to enable price transparency initiatives.
]]>
WNS has a highly developed property & casualty (P&C) insurance practice handling 30 million claims transactions and ~$12 billion in claims spend annually. The company has extensive capability in property & casualty supporting motor, property, casualty, employer and public liability for insurers, fleet operators, MGAs, global corporates, and municipal authorities. WNS has strong capability in the Lloyd’s & London market supporting specialty lines products. The company has developed a range of proprietary solutions in support of its P&C and Speciality BPM business.
The company has now taken its proposition to the next level by reinventing, automating, and digitizing its claims handling capability to assist insurers in competing with the new generation of digital disrupters.
WNS Seeking to Reengineer P&C Claims Handling to Touchless Process: Proposition – ‘Simplified Claims’
WNS’ strategy is to assist its P&C insurance clients in moving to contactless, touchless claims, with their or clients’ staff only intervening for the decreasing proportion of exceptions that need manual handling, typically for risk appetite, strategy, governance, or customer proposition reasons.
This has the potential to enable insurance companies to dramatically reduce their operating costs while simultaneously speeding up the claims process and increasing customer NPS.
For example, for motor claims, key elements in this strategy include:
- Establishing the liability for approx.70% of claims at the first notice of loss (FNOL) stage, whether received via a portal, email, or voice and then automating all downstream claims management in these cases
- Minimizing dispute timescales and costs by providing a self-serve option for the customer and third-parties to acknowledge an accident’s circumstances and share their versions of events in a timely fashion
- Automating the downstream processes if the policyholder is at fault, with third-party and subrogation interventions handled digitally
- Identifying and progressing fraud throughout its life cycle
- Handling Third Party exposures via complex AI, ML models to assess unstructured data, complete valuations, and make offers.
Similar disruptive solutions to drive high levels of straight-through processing (STP)/one-touch claims are deployed for property (personal and commercial) and casualty products.
WNS is also looking to minimize the insurance supply chain cost. For example, in property insurance, this will involve using images and video calls to cash settle more property claims at one touchpoint, eliminating the necessity for visits by loss adjustors.
Using New Digital channels for More Timely and Effective Claim Notification
One of the pain points with commercial customers and fleet companies is the amount of time taken by end customers/drivers to report accidents. In these large corporate and municipal accounts, WNS has found the average notification time to average 33 days, which leads to a loss of opportunity to intervene and reduce the loss incurred.
Accordingly, WNS is piloting the use of new digital channels so that the driver of a vehicle can effortlessly report a claim in one touch and upload images, enabling WNS to receive details such as the third party’s registration number details within minutes of the incident. This has the potential to be particularly effective in the case of drivers whose lack of fluency in English may be inhibiting accident reporting.
Similarly, for property surge events, whenever there is a warning of a weather event, such as an Australian bushfire, WNS will identify the post/ZIP codes for the areas likely to be impacted and use this new digital approach to share a prepopulated claim form with customers a day or two in advance of the weather event.
This avoids the need for customers to phone potentially heavily loaded contact centers. Instead, they upload details of their losses, and WNS will respond within 30 minutes, providing details of coverage and dispatching services accordingly.
The new digital reporting channel pilots for motor and property claims are at the completion stage and have been successful from customer experience and indemnity spend standpoints.
Enhancing the Competitiveness of a Major P&C Insurer
WNS has applied its claims strategy components to assist a major global insurer in substantially improving its competitiveness through a fundamental reinvention of its claims processes.
The insurer had carried out a competitive benchmark with a major consultancy, which estimated its OPEX to be very high on a like-for-like basis, with contributory factors being the excessive fragmentation of the insurer’s onshore delivery across more than ten onshore sites and its comparatively low usage of automation and digitalization.
WNS initially addressed these issues by consolidating the insurer’s onshore sites to two centers. WNS also made operating model changes at one of these sites, introducing a collaborative team structure with client staff working alongside WNS staff on a co-branded production floor. A WNS site head runs the site, and in addition to agents, the WNS site personnel include process leads, continuous improvement consultants, and RPA and analytics specialists. The overall client operations delivered by WNS leverage a combination of onshore and offshore delivery.
Secondly, considerable automation and digital interventions have been introduced into the insurer’s motor, property, and casualty claims process. These digital interventions are funded through an innovation funding mechanism that ensures “continuous improvement is a way of life by design”. WNS initially provided resources to deliver productivity improvements, taking a share of the resulting savings, part of which is then used to self-fund further productivity initiatives to establish a continuous reengineering cycle.
Within the new digital model, each new claim reported via the digital channel is run through an automated liability solution, followed by an early settlements, total loss, recovery, and fraud identification model, all integrated via a simple process flow running seamlessly in the background. These interventions are followed by automation of the appropriate downstream activity, such as booking the vehicle for repairs, courtesy car allotment, etc. For suspected total losses, the claim details are run through a total loss predictive tool. These processes for both repairable and total loss motor claims are supported throughout by a self-serve E-FNOL app and fraud screening.
The liability predictive model used by WNS within this contract is based on partner insurtech technology. The system automates digital liability handling within motor claims, including:
- Prompting using image-based questions to establish the accident scenario, including testimonials from witnesses, using links to Google Maps and historical meteorological data to help pinpoint the accident's exact location and weather conditions at the time
- Sending allegations to the third party for self-serve input and responses
- Integration with case law to assist in decision-making
- Built-in AI to identify fraud and subrogation opportunities.
Overall, WNS uses various commercial models ranging from FTE, transaction-based pricing, management consulting fees, and gain share within the contract. Although personal lines claims within the contract are largely paid on transaction-based pricing, WNS is additionally committed to guaranteed percentage efficiency and indemnity improvements together with customer journey improvement.
The overall benefits achieved for this insurance company included:
- Improvement of 15-20 NPS base points
- Improvement of +30 employee NPS (ENPS) base points
- ~50% OPEX reduction
- ~2% motor indemnity reduction.

Digital front doors and transparency a new normal for healthcare?
U.S. healthcare is no stranger to an environment of continuous change and has not been spared the effects of the COVID-19 global pandemic in 2020. The unique circumstances born from the need for social distancing during the pandemic have accelerated healthcare consumers' demands for digital transformation. The ask comes from all healthcare continuum vantage points – patients, providers, payers, and vendors. Healthcare must change its practices to allow for more seamless digital interactions to meet these demands.
As with other service industry sectors, healthcare consumers want the option to access their health services virtually – evidenced by an increase from an 11% utilization of virtual visits in 2019 to over 45% in 2020. Some larger health systems have made this transition without significant challenges, expanding telehealth contracts, and receiving service reimbursements for both commercial and federally funded insurance types. However, many providers were faced with the decision to either suspend their practice or invest in digital platforms or services to offer virtual visits. Cognizant's Core Admin Solutions support providers' internal processes to offer telehealth and payers and providers in efficiently & quickly submitting process associated claims and authorizations via Trizetto's Touchless Authorization Processing (TTAP). The demand for telehealth has become an independent demand from the initial catalyst of social isolation and continues to be at the forefront of patient expectations. Even the senior population is thought to have few barriers to accessing virtual care, with 84% of sampled senior consumers stating they do not have any technical challenges in attending a virtual appointment with their doctor. With the remote operation of the doctor's visit comes the corresponding demand for total digital transformation; payment processing, e-prescription writing, prescription home delivery, and remote patient monitoring. Multi-faceted companies, like Cognizant, offer a variety of bundled or unbundled services and platforms to help healthcare providers and payers address the increased demands for digital interactions. This new digitization is also thought to reduce costs by increasing care coordination, administration, and manufacturing efficiency.
Providers and Payers are finding that digital products also offer the opportunity to clinically manage their patients and members remotely, with IoT, remote monitoring devices, and health wearables. The consumer can utilize various devices, measuring vitals, health coaching through AI, and tracking other metrics related to health risk factors. 65% of consumers utilize some type of wearable. With this percentage of adoption and available data, providers and payers have an exciting opportunity to address their patients' and members' health outside of the doctor's office. Vendors offer bundled platforms or paired digital services to collect, aggregate, and analyze the patient/member data to facilitate care management efforts by both their clinicians and their health plans. Though this digitization also requires a financial investment from the organizations, the vendors promise a visible ROI in cost savings and improved health outcomes.
Driving the transformation
Regulatory bodies have been pushing healthcare providers and payers towards a digital transformation, most recently with the ONC Cure's Act Final Rule. The rule was created to increase interoperability and access to consumer's own health information. Though the rule pushes providers and payers towards the shared goal of an enhanced patient experience, compliance with these requirements will come at a cost. By 2021 payers will be required to allow consumers access to all their claims and health information and to develop APIs to share data with other organizations and regulatory bodies. Though the compliance will be a financial investment for providers and payers, vendors such as Cognizant can implement or offer platforms to achieve such price transparency.
The Centers for Medicare and Medicaid Services (CMS) has similarly taken steps to guide providers and payers towards a better patient experience. In the 2021 Medicare Advantage Final Rule, CMS announced a change to its CMS Star Ratings measures, increasing the weight of the patient experience metrics. Payers must now invest more heavily in their consumer requirements – digital transformation to achieve an end-user-friendly suite of digital platforms. Cognizant addresses another of these drivers by offering several applications and platforms that facilitate both back-end processes and consumer-facing platforms in assisting payers in meeting heightened digital demands from their consumers. Cognizant's continued investment in Trizetto products offers payers such an opportunity for an enhanced user experience with an automated enrollment platform. Such an offering would make a payer more attractive in the upcoming Medicare Advantage and ACA Marketplace OEP (open enrollment period).
Healthcare organizations are also feeling the pressure for change from InsurTech companies and their partnerships with healthcare providers. These initiatives are attracting members and patients with their omni-channel user interfaces and strategic focus on digital platforms and processes.
Product Suites to Achieve the New Normal
Amongst Cognizant's comprehensive suite of product offerings, their digital healthcare platforms and services support over 200 million lives in the U.S. Payers and providers alike have the option to select a la carte products or bundled services to meet the changing regulatory requirements and evolving demands of their consumer and patient bases. Cognizant continues to exact leadership and be forward-thinking in its current and planned digital transformation offerings and continued investment in Trizetto Healthcare Products ($100m):
- Core Payer and TPA admin solutions, for claims processing and management
- Payer-provider solutions, for facilitating contract pricing and modeling and payment administration. Cognizant has planned offerings for onboarding and credentialing
- Government and Quality Solutions, for enrollment and encounter data management, and support of quality rating measures and reporting. Cognizant is planning offerings for enhanced care coordination
- Care Solutions, for clinical and utilization management and value-based benefits. Cognizant is planning offerings for for automated authorization and referral management
- Data orchestration SoE solutions for data aggregation and engagement. Planned offerings include additional integration and analytics for interoperability.
While Cognizant, and other vendors, offer a wealth of products and platforms for health systems and payers, for many the financial investment required has been a barrier. But COVID-19 is having an impact, in spite of an estimated four-month loss of $202.6bn for hospitals and health systems in the U.S. Every U.S. health system recently interviewed by NelsonHall regarded digital transformation as more important as a result of COVID-19, with increased investments planned in SaaS and cloud infrastructure. Overall, hospitals & health systems in the U.S. have shortened their planning horizons to address short-term priorities and investments. One major healthcare system stated that their planning horizon was now weeks rather than years. The same reduction in planning horizon is also evident in healthcare payers, but here with a need for customer retention combined with a much stronger emphasis on cost control.
As is true in other sectors, the pandemic will likely increase the acceleration of digital transformation initiatives across healthcare, with a clear focus on achieving short-term results (rather than in years), producing very immediate improvements in both productivity and customer experience.
]]>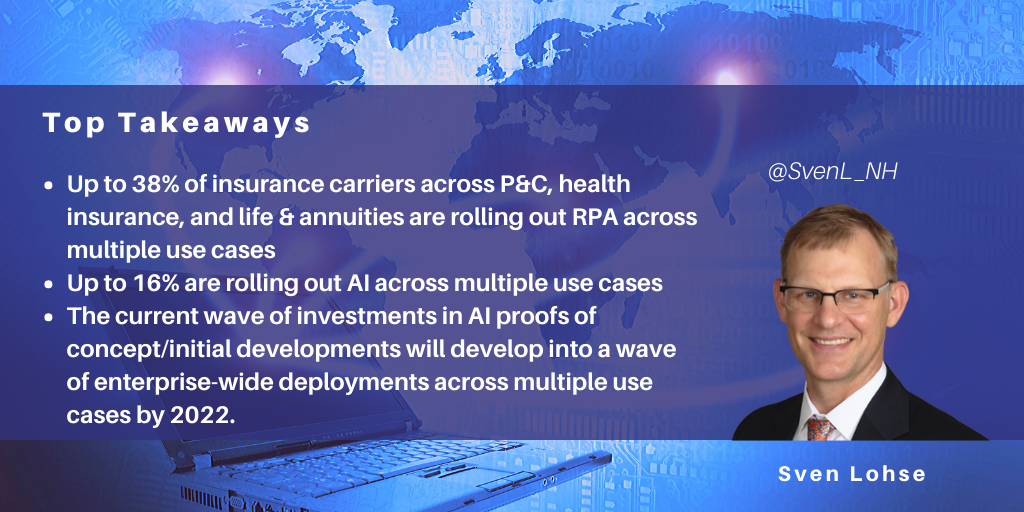
NelsonHall predicts that by 2022, 35% of insurance industry carriers will be in the process of adopting AI technology across multiple use cases within the enterprise. This is based on NelsonHall survey data from the insurance industry that tracks adoption of both RPA and AI (NLP/ML/DL) technology across the property & casualty, health insurance, and life & annuities insurance sectors.
Survey findings
Between 31% and 38% of surveyed carriers are beginning to roll out RPA across multiple use cases, while between 3% and 16% are beginning to roll out AI across multiple use cases – this range includes P&C (3%), L&A (4%) and healthcare payers (16%).
We expect a similar rate of maturity development for AI as for RPA. For RPA, we have seen a wave of investments in proofs of concepts/initial deployments in 2016/2017 develop into enterprise-wide initiatives in 2019/2020. We expect to see the current wave of investments in AI proofs of concepts/initial developments to develop into a wave of enterprise-wide deployments across multiple use cases by 2022. As was the case with RPA, we see a wide variety in the rates of adoption for different types of AI (in particular for natural language processing, machine learning, and deep learning).
The business functions that lead in adoption of AI include:
- P&C insurance: policy origination, underwriting automation, and capacity to manage changes in volume of customer interaction in real-time
- Life & Annuities: policy pricing optimization, contact center real-time customer support, investment support
- Health insurance: product pricing optimization, marketing decision-making.
AI adoption will likely reflect the following broad trends:
- U.S., U.K., and Asia/Pacific carriers will in general lead their counterparts in Continental Europe in the implementation of AI
- Some business functions will provide more fertile ground for adoption of AI, e.g. personal lines insurance policy origination, and customer service will continue to adopt AI more quickly
- Continental carriers will emphasize the importance of customer service and increased speed/ease of new business acquisition in comparison to straight through processing, which is more frequently the top priority for U.K., U.S., and Asian carriers.
General guidance for carriers in adoption of AI
Enterprise governance
Effective enterprise-wide rollouts and scaling of new AI technologies will require strong enterprise governance structures. Efforts completed on behalf of similar enterprise deployments of RPA will pave the way for AI adoption. See the following NelsonHall blog for an example from the health insurance industry: How NTT DATA Established Enterprise Automation Governance for BCBS Health Insurance Carrier
Adapt roles and skills within personnel pyramids
Adoption rates and effectiveness of implementation of AI technologies will ultimately depend on the organizational structures and quality of the people used to transform carrier operations. Carriers will therefore be required to redefine organizational structures, roles and skills. (This will be true whether AI adoption is conducted with or without the extensive use of external consulting and/or outsourcing partners.) Expect significant lag time between the articulation of new organizational structures, roles, and skills, and the period in which enterprises can acquire talent. As with most new technologies, AI experts will be hard to identify, attract and retain, whether compensated directly by a carrier or not.
Align with existing procurement strategies
Procurement strategies that manage external AI partner vendors need to be clear, manageable, and adapted to enterprise procurement structures in place. It’s noteworthy that while outcomes-based, or gain-sharing, contracts get a lot of attention, about 90% of P&C transformational outsourcing contracts in the U.S. are still managed on an FTE, fixed-price, or transaction basis. In Asia Pacific, that proportion is even higher. So, especially for early-stage AI projects, insurance carriers should likely consider keeping outsourcing contracts as straightforward as possible.
Get early buy-in
Winning the race to effective, enterprise-wide adoption of a new technology frequently depends on how innovators introduce that technology within the context of the enterprise. Far-sighted planning may include pilot projects that start small, and then earn organizational buy-in based on clearly demonstrable, early wins. Employee upskilling programs can help allay the fears of those concerned with being displaced by new technologies.
]]>
A magnitude-6.4 earthquake struck Puerto Rico on January 6, killing one person, toppling homes and buildings, and triggering a blackout on the island that is still recovering two years after Hurricane Maria. Governor Wanda Vázquez declared a state of emergency and activated the Puerto Rico National Guard to help with recovery efforts.
How might this earthquake disaster have affected delivery of outsourcing services from Puerto Rico (P.R.) to U.S. clients? Infosys’ response to the devastation caused by Hurricane Maria sheds light on whether the buyers of nearshore outsourcing services should expect significant interruptions to service as a result of such natural disasters.
Infosys’ Puerto Rico delivery center
In 2013, understanding Puerto Rico’s risk exposure to natural disasters, Infosys set up a delivery center in Aguadilla, P.R., as part of a deal to optimize global operations for a client Fortune 500 consumer, engineering and aerospace technology company. Advantages from Infosys’ point of view included:
- Local knowledge: prior understanding of the local Aguadilla business environment through its work with the client
- Rafael Hernández International Airport: located near the delivery center, the transportation hub supports a local aerospace industry that sustains a reservoir of local IT and knowledge services skills
- Skilled local outsourcing professionals: P.R. residents enjoy the full rights and legal protection of U.S. citizenship (P.R. is an unincorporated territory of the United States); they tend to be multi-lingual in both English and Spanish, and tend to be inexpensive compared to counterparts in the mainland U.S.
- Tax relief provided under P.R.’s Economic Development Incentives Act: “the cost structure was a little more amenable in comparison to some of the other locations in the U.S.,” said Aniket Maindarkar, head of Infosys’ Americas operations at Infosys BPO, in 2014. The Puerto Rico Industrial Development Company (PRIDCO) offered a 100% exemption on taxes on earnings and profits, and a 90% deduction on local property taxes. PRIDCO’s executive director Medina explained at the time that “although [P.R. is] part of the U.S., we can negotiate tax rates with companies and they do not pay federal tax rates”
- Staff training and other aid: PRIDCO helped train staff and aided Infosys in finding a new facility location
- High profile political support: Infosys’ investment in a P.R. outsourcing delivery center garnered press exposure through the P.R. Governor’s visit at the opening of the new Infosys facilities in Aguadilla.
Disaster resiliency features
At the time Infosys initially established nearshore outsourcing capabilities in P.R., the company publicly announced it envisioned serving U.S. clients in multiple restricted industries, including defense and healthcare. Within a year Infosys had relocated both retained and new personnel into a nearby 12,000 sq. ft. facility that could accommodate up to 300 people. The relocation retained features that would later prove advantageous to disaster resiliency, including:
- Aguadilla’s location on the northwestern side of P.R. helps protect facilities from strong winds and hurricanes that tend to land on the eastern and southern sides of the island
- The local Rafael Hernández International Airport is supported by the infrastructure of a former U.S. Air Force base and is located less than ten kilometers from Infosys’ Aguadilla facility
- The airport offers direct commercial flights from multiple airlines to the U.S. mainland, including the greater New York City area. This is the location of a major Infosys healthcare outsourcing services client served by its Aguadilla personnel
- Backup electrical power, supplied by diesel-powered generators located at the Infosys facility.
Expanding capabilities to the healthcare sector
Since 2016, Infosys has expanded the capabilities of the delivery center from aerospace industry functions to operations in the communications and healthcare industries. For U.S. healthcare clients Infosys began to build out clinical and IT service desk and support for Medicaid business. Initially, Infosys hired half a dozen P.R. clinical nurses with both bedside and corporate/investigative expertise.
The U.S. legal status and U.S. citizenship of the P.R. personnel supports delivery of restricted defense industry and healthcare industry services (e.g. Medicaid program services) with lower local costs than those of U.S. counterparts. According to U.S. Bureau of Labor statistics, median wages for registered nurses in the U.S. are approximately double those of their counterparts in P.R. However, among the nurses with both bedside and corporate/investigative experience that Infosys recruits in P.R., Infosys’ experience is that the discount for clinical nurse labor rates is narrower: 15-20% discount for a nurse in P.R. compared to New Jersey, and 10% discount for other highly skilled resources.
Lessons from Hurricane Maria
When the Category 5 hurricane hit Puerto Rico in September 2017, it lingered over the island for over two weeks, causing over $90bn in damage and approximately 3,000 fatalities. Nevertheless, despite the scale of the devastation, Infosys reports that its service to clients was interrupted only for one day while it implemented its disaster recovery processes. Diesel generators supplied power to employees for the duration, and most employees resided in the facility rather than go home when off duty. Infosys also retained transportation links with its clients. Despite the atrocious weather, Infosys secured approval to fly by private jet into Aguadilla’s airport on an emergency basis and flew some of its P.R. personnel to client locations in the mainland U.S. Infosys also used these flights to transport vital physical supplies and even cash for salary payments to its Aguadilla personnel.
Through the Maria event, Infosys learned that its communications links required further improvement. Deployment of satellite links into Infosys’ global IT network now enable resilient communications and internet connectivity independently of local fiberoptic and telecommunications infrastructure.
Infosys’ responses to the Maria event have reassured healthcare clients that its facilities in Aguadilla are adaptive and resilient in the face of major natural disasters. Since 2017, Infosys’ outsourcing services from Aguadilla to mainland U.S. clients have expanded, and in the last year Infosys reports that it has expanded clinical healthcare outsourcing services to a second U.S. health insurance company. Infosys now employs approximately three dozen nurses at the Aguadilla facility. Infosys is prospecting for more clients, and has developed contingency plans for bringing other Aguadilla facilities online should a major client win exceed current excess capacity of approximately 60 seats.
]]>
Convex Group is a start-up specialty insurer and reinsurer focused on complex risks, launched with $1.8bn of committed capital in April 2019. Convex will underwrite insurance and reinsurance for “complex specialty risks across a diversified range of business lines” in London and Bermuda. The company aims to adopt a conservative investment strategy with a predominantly high-grade fixed income portfolio and duration matched to the profile of the liabilities.
Development of an Insurance-in-a-Box Operating Model
As a start-up, Convex had no legacy infrastructure or operations and was looking for an “out-of-the-box” insurance and reinsurance infrastructure and operations model, priced on a per transaction basis to enable it to achieve a new level of cost ratio performance.
Accordingly, Convex evaluated multiple vendors against three criteria:
- The extent to which each vendor could align on their operating model and provide an “insurance-in-a-box” offering
- The detailed service model and the ability of the vendor to underpin this model with technology
- The ability to mobilize experienced personnel quickly and execute in a short timeframe.
Following this evaluation process, Convex signed a long-term strategic partnership with WNS in April 2019. The key factors that differentiated WNS following discussions and site visits by Convex in Pune, India included:
- Their depth of insurance industry domain expertise and scale of investment in the industry. WNS has extensive experience in working with global specialty insurers and reinsurers and brokers
- Their service excellence and risk management focus
- Their flexibility in adapting to Convex’s requirements at speed.
WNS has subsequently created a onshore/offshore target operating model and has successfully implemented the technology stack in the initial start-up period of 6 months to manage the HR, Finance and Accounting services, and multiple Industry-specific activities including claims processing, and inward (re)insurance underwriting support. Convex will largely deliver product development and underwriting.
The technology being used is Sequel insurance software, already implemented in support of underwriting, with Oracle cloud software implemented in support of HR and accounting.
WNS Free to Offer Solution to Other (Re)Insurers
With this contract eventually aiming to move toward a per transaction pricing basis, WNS is banking on substantially increased revenues from the contract as Convex becomes established and captures market share in the reinsurance sector, with both Convex and WNS perceiving that the resulting lower cost from this new operating model will provide a source of competitive advantage. Indeed, Convex perceives that by using WNS and this operating model, it will be able to target a cost ratio of 10%-11% rather than the 13%-15% typically achieved.
Convex believes that as a first-mover and start-up with no legacy baggage it can derive greater short-term advantage from this solution than its established competitors, though WNS is free to offer the “insurance-in-a-box” solution developed for Convex to other (re)insurers and sees this as a major new market opportunity as insurers look to reimagine their operating models.
]]>
Dozens of influencers recently attended the WNS U.S. Influencer Day in New Orleans, where the theme was 'Co-create to Outperform’. Through general overviews of its approaches and through client presentations, the company provided insight into its recent success and its future plans. The backdrop for the conference was cheery, buoyed by 7% annualized growth over the prior fiscal year.
Here I look at a couple of highlights from the event, focusing on WNS’ healthcare business and at its approach to business transformation generally.
Healthcare domain expertise
HealthHelp, a company WNS acquired in September 2017, has become the central pillar of WNS’ healthcare business. HealthHelp was likely much larger (NelsonHall estimates >$40m in revenue) than the extant WNS healthcare segment business at the time, hence it is likely HealthHelp became the core around which WNS organized the rest of its healthcare business. Potential integration problems seem to have been avoided by granting HealthHelp a long leash; HealthHelp remains branded as “HealthHelp, a WNS Company”. Both the acquired and the acquiring companies appear to be learning from each other. The broader WNS business may be adopting some of HealthHelp’s approaches to supporting services with proprietary software. HealthHelp’s proprietary software platform reportedly supports the stickiness of its services, and WNS is contemplating ways in which it can further support client services in other verticals using similar proprietary software platforms.
Houston, TX-based HealthHelp provides the foundation for healthcare revenue that is now approaching or exceeding 15% of total WNS revenue. The healthcare vertical anticipates double-digit growth in 2019. WNS’ “non-denial” clinical services enable payers to support providers within its network to provide optimal, cost-effective care. WNS facilitates educational, supportive interactions that enhance provider satisfaction rather than a confrontational or abrasive interaction that degrades provider satisfaction. WNS does this by bringing expert staff from its network of clinical specialists at academic medical centers into conversation with its providers in order to resolve cases that have been determined by the payer or by WNS to be inappropriate for any reason, clinical or economic.
The company’s value proposition and strategy appear directionally unchanged, although more may develop in this regard following the recent promotion of Kariena (Zacharski) Greiten to the role of CEO for HealthHelp. Prior to this promotion, Greiten had been Chief Product Officer at Magellan Healthcare.
Transformation approach
The Co-Creation theme of the conference (and of WNS marketing) was expounded by WNS executives such as Adrian McKnight, EVP of Transformation and Quality, who said “We look to be a transformation partner rather than an outsourcing partner.”
WNS believes that perspectives on outsourcing are maturing. Initially, potential clients may consider outsourcing a piece of the value chain. But if they don’t begin with an end-to-end analysis of what the business could deliver to the end user, they begin to ask “What is beyond the KPIs of the outsourcing contract? What are the broader operating and business models required to facilitate the customer journey?” Then companies realize they are looking to buy transformation, not outsourcing. While outsourcing can be an aspect of a solution, it may not be the core requirement.
Domain expertise such as that which WNS offers through HealthHelp creates opportunities for WNS to take a seat at the table in discussions with clients on how to realize digital transformation. An intimate understanding of a healthcare payer’s organization helps immeasurably as WNS assesses the potential for transformation.
The iterations required to plan, build and implement client solutions rely on good collaborative practices, which, in turn, are founded on IT agile methodology. In WNS’ view, IT “agile” has matured to become a more holistic set of practices that integrate the functional needs of the client organization from all areas, not just IT. WNS claims to focus heavily on this broader view of the strategic position of its clients because culture and the speed of agility depend on this contextualized perspective. These eventually drive IT development projects and outsourcing contract requirements.
As WNS works through business problems with clients towards appropriate solutions, the ultimate success of WNS Co-Creation relies on the relevance and meaningfulness of its capabilities. Speed is also of primary significance. Whether those capabilities are supplied internally by the WNS enterprise or via its network of partners, WNS aspires to remove friction and increase the speed at which it can cycle through iterations, particularly in the implementation phase of a Co-Creation experience.
]]>
In this blog, I look at how NTT DATA worked with a large Blue Cross Blue Shield (BCBS) health insurance carrier to establish an enterprise governance structure for automation, and at the lessons learnt along the way.
Like many other large BCBS carriers, the company had piloted RPA initiatives, and from the somewhat frustrating results of these experiments, it had formed two conclusions:
- An IT department-driven center of excellence delivering bots will not achieve the full potential of automation
- Point solutions being driven within individual towers/business units are not scalable across the enterprise.
The company concluded that before it could proceed with its automation journey, it required an automation governance structure that aligned with the enterprise strategy. A business-driven (rather than IT-driven) deployment of RPA needed to coordinate the needs, requirements and deployment of RPA across the front, middle and back office functions, as well as shared and internal ancillary services.
The BCBS carrier hired a team from NTT DATA, led by Deana Rhoades, the Global Practice Lead, Healthcare Automation “to create an enterprise-wide governance structure customized to their corporate strategic objectives and organizational culture”. Within the context of the enterprise’s goals, strategy, and current workforce, the company tasked NTT DATA to create the automation strategy, the decision frameworks and the organizational structure. While the BCBS company had long before established solid objectives, frameworks and management systems for its human workforce, the company realized it needed to lay the foundation for the same kind of structure for automation (and the bots) of its “digital workforce”.
Starting in August of 2018, NTT DATA began its work creating an enterprise level governance structure for automation. It focused on scalability considerations and governance, treating bot development “almost as an afterthought”. The tactical view about how to purchase and deploy automation solutions and build bots on different platforms would flow from the enterprise’s strategic objectives and from appropriate integration of the human and the proposed digital workforces. It took two months for NTT DATA and its client to articulate the following governance model, composed of three layers:
Layer 1: Sponsorship
Champions of the RPA transformation articulated the vision and goals for the automation journey and monitored performance of the COE. Sponsors include high-level representatives of the COO, the CIO and the HR departments, coordinated by a Program Management Office (PMO). Strategic frameworks now articulate the enterprise’s objectives, categorize potential automation projects within that context, and facilitate decisions about deployment in terms of (for example):
- Potential cost savings (prioritized over revenue)
- User experience (prioritized over productivity).
Layer 2: Enterprise Capability Center
This team unites leaders and dedicated resources from the following functions: HR, Data and Analytics, IT, Security, Organizational Change Management, Business Process Management, and Operations. Six workgroups develop and provide expertise on the core COE capabilities. The COE subgroups cascade the automation strategy into action plans that provide capabilities across automation development teams and business units. Focus areas include:
- Strategy and Measurement – turns strategy into executable components; owns success criteria, key performance indicators (KPIs) and objectives and key results (OKRs); quantifies the value of the COE
- Pipeline Management – generates demand for automation at the process level among BCBS company employees, prioritizes and schedules the resulting workstreams
- Workforce Strategy – defines needed FTE skills and gaps, owns the organizational change management (OCM) plans and provides training for BCBS company employees
- Automation Standards – develops the standards, tools, repositories, policies and procedures that guide all automation initiatives
- Data Strategy – maintains data management strategy, defines how automation software accesses and collects data, and how the automation efforts comply with risk and security policies
- Virtual Workforce Monitoring – maintains a centralized command center to monitor and oversee the bots in production.
Layer 3: Automation Factory
Delivery and deployment teams work under the aegis of the leadership priorities and plans developed in layers 1 and 2 with complementary aims:
- Demand generation – generating awareness and demand for automation within the enterprise at the level of the teams that manage specific processes. A change management team trains these teams on capabilities of RPA and helps them see the value of implementing the technology
- Technology delivery – agile development teams automate processes using the appropriate tools and platforms, such as Blue Prism and UI Path.
For the next phase of work, NTT DATA has begun to create a complementary hybrid (or “federated”) operating model for agile delivery of bots. This hybrid model is supposed to establish the guardrails and frameworks needed by individual business units that have the skills and the desire to build their own bots. The hybrid model is expected to augment the centralized enterprise governance model by 2020.
The human response?
With NTT DATA, the BCBS company has worked to communicate with various business units and with their leaders to resolve their questions and any potential anxiety about the use of bots. During the BCBS company’s prior work with another IT consulting firm, it had developed its own home-grown automation tools. The in-house deployment of an RPA platform had introduced the company to concepts and practices at a tactical level. Activities surrounding these pilots had been widely broadcast through various communication channels, including robotic roadshows, Yammer, and email. As a result of this in-house publicity, NTT DATA reported that it met with more curiosity and less resistance than expected. NTT DATA also reported that company business units and employees had already begun to form opinions about automation through the lens of their experience with their prior RPA tool, opinions that needed to be considered if and when other development tools were introduced.
The business consequence?
NTT DATA believes that the BCBS carrier has taken a significant stride up the automation maturity curve by articulating a governance model with the following elements
- Charter
- Roles and responsibilities
- Leaders
- Change management
- Resources dedicated to organizational communication and demand generation
- Resources dedicated to development of a broader set of intelligent automation technologies.
RPA initiatives that predate the NTT DATA-led exercise in defining automation governance now have a structure and resources available when they need to escalate issues, and have realized greater ROI. Furthermore, the BCBS carrier’s “ox in the ditch” initiatives have now been organized into six workstreams, and in future the company believes that its governance structure and measured approach will yield expected ROI and that its human and virtual workforces will complement each other efficiently.
]]>
In my previous blog, I described how, since 2017, Sutherland has created a shared services model that obviates the need for participating California health plans to separately build and update parallel databases to track the availability of providers of nonurgent care for Medicaid recipients.
The company estimates that through its consortium of member health plans it has reduced associated health plan physician data management costs by 75% through elimination of duplicative work and by improvement in survey execution workflow and other areas. For an estimated 80,000 physicians in its CA directory, Sutherland now estimates that it reduces the touch rate on providers related to the Provider Appointment Availability Survey (PAAS) from three to one call per practice. The initiative also improves reporting and other interactions with the California regulatory body (Department of Managed Healthcare, or DMHC) and improves patient access to timely care.
Sutherland’s success with its coopetition/shared services model begs an interesting question: can this model be extended across the U.S. and, if so, how?
Uncovering value from duplicated effort
The coopetition model now proven in California might provide a useful template for future work at the national level. Data from Sutherland’s efforts in California indicate that national health plan provider networks significantly overlap and that much of the work they pursue in building and maintaining their physician databases is therefore duplicative and wasteful. In California, Sutherland reports a 48% overlap of providers between the top three CA health plans. That is, of ~20,000 physicians that are currently contracted to plans managed by one of the top three health plans in CA’s Medi-Cal Medicaid program, over 9,000 are currently contracted with all three health plans. Each health plan in California is required by the DMHC to maintain accurate data on each provider so that patients can gain access to timely care. Each health plan is further required to manage this dataset in order to maintain its own operations. The difficulties in maintaining these parallel datasets result in a myriad of problems for different stakeholders, including wasted effort.
Stakeholders include vendors of business outsourcing services. Prior to Sutherland’s involvement in the shared services initiative, the data collected by the DMHC was of such poor quality that it resulted in a directive to all CA health plans saying that the vendor then in charge of managing the provider data collection effort would no longer be allowed to work in CA.
Sutherland reported that, at that time, 40% of data records contained errors or omissions. The result was that health plans could not confirm members for timely and appropriate access to care, and providers were subjected to unnecessary inconvenience, cost and fatigue. The opportunity for a vendor of business outsourcing services, conversely, was significant. Since two-thirds of data collection efforts by different health plans required the same basic information from providers, Sutherland identified an opportunity in California to generate value by eliminating unnecessary work and collecting a slice of the resulting value, while simultaneously providing value to the regulatory body, providers, and patients.
Geographic & market segment extension of the model
The geographic extension of this model in physician network data management beyond California may be a logical next step. Sutherland itself calls its shared services model for the provider appointment availability survey (PAAS) a “proof of concept”. The fact that Sutherland has successfully united the interests of competing health plans with those of providers, patients, and the state regulatory body lends credence to the idea that other health plans in the U.S. might be convinced to join a similar consortium. Note that some health plans would likely never be candidates, such as Kaiser Permanente, which is based on a vertically integrated model that unifies the management of provision and reimbursement of care. (While Kaiser provides Medicaid services in California, it is not a member of Sutherland’s current shared services model in CA).
However, whether led by Sutherland or another entity (private or public sector), such a consortium could eliminate waste on a state-by-state basis, or even more broadly. The model could be extended to other government healthcare. It could standardize and streamline data collection, present accurate data to a wide range of stakeholders in timely fashion, standardize reporting, reduce provider fatigue significantly, and improve customer/patient access.
Generating leverage
Creating a public utility by mandate may lead to inefficient, unintended consequences, but Sutherland’s success seems to indicate that a market solution can be viable. The CA consortium currently counts 14 health plans, but replicating this success outside CA would require customization to other economic and political circumstances. The mission of the Council for Affordable Quality Healthcare (CAQH) and other associated alliances, non-profits, and government agencies may align with such efforts. Companies that specialize in providing outsourcing services have, as Sutherland proves, many of the capabilities required. Short of a government-sponsored mandate, how can health plans be induced to share proprietary data and data methodologies?
Political leverage might be hard to generate among consumers/patients, but physicians may present a more unified and sharply-focused interest group. If a doctor contracts with a single health plan for multiple products (e.g. Medicare Advantage, Mental Health, etc.) and that doctor’s information needs to be verified for each product, this would require multiple touches, cost, inconvenience, and fatigue. According to Sutherland’s experience in CA, that doctor may, on average, contract with 20 health plan products. The doctor is therefore incentivized to reduce this duplicative and wasteful interaction, and the argument that physician rosters can be harmonized among health plans with minimal interaction (leveraging web portals rather than call centers) is not hard to make. Having thus grasped the challenge, the physicians’ professional organizations may be well-placed to work with health plans to set up more consortia similar to Sutherland’s in California.
Finding allies
An industry alliance designed to introduce blockchain is aimed directly at the challenge of reducing the estimated $2.1 bn in cost associated with maintaining provider data. According to an April 2018 healthcareITnews.com article, Optum, UnitedHealthcare, Humana, others launch blockchain pilot, these industry titans are exploiting the opportunity to reduce waste associated with provider data: “Five healthcare organizations including insurers UnitedHealthcare and Humana, Optum, Quest Diagnostics and MultiPlan are launching a blockchain pilot to help payers tackle mandated provider directories”.
The mission of this alliance may provide a long-term objective to which one or more consortia based on the Sutherland CA model might be mutually supportive. The hype associated with blockchain might create the attention necessary to establish more provider data consortia, while the political clout of physicians’ professional organizations might bring leverage. In combination, private sector players might then find the resources and support necessary to align economic incentives, manage workflows, normalize and de-duplicate data, execute against state and federal regulations, and package provider data in digestible, accurate, up-to-date formats for the constellation of healthcare stakeholders.
]]>
Benefitfocus, the cloud-based benefits management platform and services provider, recently hosted 1,200 benefits professionals at their annual One Place conference in Charleston, S.C. The conference featured updates on Benefitfocus’ strategy, enterprise benefits management technology platform, and partners from its ecosystem; and presented an opportunity to learn from industry thought leaders, technology partners, benefits suppliers, and insurance brokers. On the final day of the event the company facilitated employer efforts to build benefit strategies and experiences at what was billed as the industry’s “largest open enrollment planning event”.
During the event, Benefitfocus updated customers and ecosystem partners on seven key topics, as covered in this blog.
Shift in corporate strategy
Benefitfocus has embarked on a significant strategic realignment. The company is shifting its company strategy from selling software to facilitating a benefits industry platform (or marketplace, such as Amazon). The company has been influenced by the book Platform Revolution, written by MIT professor Geoffrey Parker, who was introduced via a recorded video after having visited the company at its campus headquarters in South Carolina. Parker’s book instructs leaders how to start and run a successful platform business such as Amazon, explaining ways to identify prime markets and monetize networks.
Benefitfocus’ ambition is to “connect benefits buyers and sellers in unprecedented ways” and be accepted in a new bracket of peers, including Amazon, airbnb, and Uber. In practical terms, newly introduced analytics are designed to allow sellers and brokers using Benefitfocus’ SaaS software to segment employer customers and employee populations for “improved benefit strategy, communications and engagement, while giving employers robust visual interactive tools to quantify the value of their benefits programs and serve their employees.”
However, questions regarding the practical ramifications of this strategic shift remained unaddressed in the general sessions, including:
- The shift from a software development culture habituated to a standard, planned software roadmap and update release schedule to a “platform” culture habituated to agile development
- Adaptation of the Benefitfocus sales channel, sales methodology, sales collateral, sales and marketing resource roles, responsibilities and staffing
- Development of an ecosystem partnership within a complex web of coopetition (in which medical carriers, for example, may currently go to market on the Benefitfocus SaaS software, white label Benefitfocus, and/or go to market concurrently with their own home-grown development platforms).
- Development of the benefits administration professional community within Benefitfocus’ ecosystem of employers, consumers, and benefit providers.
Software updates
Benefitfocus platform updates that resonated strongly with benefits partners included:
- Mobile App: It is now possible to email or text health data to a physician, including proof of insurance. This is a service not only for the consumer but for the insurance carrier that wants to have accurate data conveyed to physicians in real-time. The Mobile App aims to simplify consumer engagement, total rewards details, and digital ID cards. Enrollment can now be accomplished using the Mobile App.
- Chatbot: Embedded in AI engine BenefitSAIGE, this 24-hour chatbot drives content and recommendations to consumers every type of benefit at every stage of life. It also frees the HR professional who is ordinarily called to interface with consumers about the benefits platform and benefits companies. Chatbot communications limit delays generated by hand-offs as a consumer inquiry passes to the HR professional, to a benefits broker, to a benefits vendor, and then returns back to the HR professional and finally the consumer. The chatbot also drives appropriate benefits enrollment in “smart moments” that matter to consumers.
- Digital Wallet: This feature enables flexible payment options beyond payroll deduction. Payment using personal credit cards can also be accomplished using the Mobile App. The platform now allows employees to purchase insurance at any time during the year, not just during a two-week open enrollment period.
Other notable added software functionality includes:
- Data interchange and automation enhancements, analytics and communications enabled by AI engine BenefitSAIGE. The AI engine leverages rules-based systems, RPA, machine learning, predictive analytics, and natural language processing. This AI engine aims to improve data interchange, drive insights, improve the consumer experience, and influence transactions during “smart moments”
- Ecosystem productivity enhancements via data exchange, APIs and automation, supported by security and data protection.
Benefitfocus reports that over 25m consumers are now served by its software platform. Clients include 170k+ employers, from Fortune 500 companies to small employers, featuring 17k brokers, 144 medical benefits carriers, and 30+ marquee voluntary and specialty benefit brands.
Data cleansing
The company reports that a $30m investment has produced a dataset with “99.6% data accuracy on first-pass yield, eclipsing the industry average of 95%”. The dataset includes records of 2.7bn data transactions in 2018 alone.
Adding a portable life insurance partner
BenefitsPlace now features Afficiency, an InsurTech that is working with life insurance carriers to offer portable voluntary life insurance benefits.
Adding consumer-directed health partners
The company has also added greater choice of consumer-directed healthcare (CDH) account options, including Wageworks and Payflex. API connections are designed for synchronized, accurate and real-time data exchange. Year-round education and communications should help consumers maximize their CDH contributions, including the triple-tax benefits of funding their HSAs.
Introduction of personal lines insurance products
On the existing software platform, insurance carriers and specialty product suppliers gain a dedicated digital distribution and enrollment channel to more than 23m consumers on the Benefitfocus platform. Carriers included in this first iteration include:
- Bristol West Insurance Group: a member of the Farmers Insurance Group of Companies (PL auto)
- MetLife Auto & Home: Metropolitan Property and Casualty Insurance Company and its subsidiaries, operating collectively under the MetLife Auto & Home brand (PL auto and homeowner)
- Toggle: launched by Farmers Insurance in 2018 (renter’s insurance).
Benefitfocus offers P&C insurance through licensed brokers at discounted rates.
Innovation incubator
Benefitfocus announced its InnovationPlace, a startup partner program. The company aims to introduce innovative products and services to employers and their employees through its SaaS facilitated marketplace. The company has created an innovation incubator on the company’s South Carolina campus, and welcomed its first occupant, Rock Health, an innovator in women’s health.
]]>
In this blog, I look at how Sutherland tackled the challenge of health plans maintaining accurate provider data in the state of California.
The challenge: inaccurate health plan data about providers
It’s been difficult for health plans in California to maintain accurate, up-to-date information on the current status of providers in the state. According to outsourcing vendor Sutherland, experience indicates that 60% of provider directories contain serious material errors. Health plan data frequently indicated that doctors were no longer accepting new patients, even though they in fact were. The data frequently presented the state regulatory body, health plans, and patients with inaccurate information about whether doctors continued to practice their specialty, had moved to new locations, or were contracted to work with particular health plans or their products.
The context: gaining access to timely CA medical services
Since 2017, Sutherland has created a shared services model for over a dozen CA health plans that obviates the need for participating California health plans to each separately build and update parallel databases that track the availability of provider appointments for urgent and non-urgent care for health plan members. The State Department of Managed Healthcare (DMHC), which regulates the state’s health plans, requires that health plans and providers make available appointments for urgent and non-urgent care, varying by specialty, from two to 14 days. Until recently, each health plan created and updated its own massive database of providers that participated in each of those plan’s products.
In a state in which Sutherland reports that the average provider contracts with ~ 15 health plan products, the law resulted in a myriad of duplicative efforts, each of which imposed burdensome requirements on providers.
The Sutherland solution
Sutherland has initiated a shared services platform that reduces this burden for health plans, providers, and state agencies, and increases the accuracy of reporting to the DMHC. In particular, Sutherland spearheaded the coopetition of health plans in California in 2017 by creating a shared services model that built and updated the Provider Appointment Availability Survey (PAAS) on behalf of a consortium.
Prior to that, Sutherland had been in conversations with the state of California on a related topic, and that conversation helped initiate Sutherland’s PAAS project with the state. Sutherland had already built a relationship with Blue Shield of CA, which became the anchor client. Other state-based and national health plans joined the consortium in 2017, totaling eight by the end of 2017. By the end of 2018, 12 health plans had joined the consortium and Sutherland now counts that consortium at 14 health plans.
Sutherland estimates that it now touches ~ 100K doctors, each of which has contracts with an average of two plans. This hub-and-spoke shared services model eliminates duplicate outreach to CA providers, saving each participating health plan from the costs of maintaining separate call center facilities and databases, and saving providers from responding to multiplicative health plan outreach regarding the same basic data. Sutherland also manages all the workflows involved with credentialing a new provider, verifying diplomas, board certifications, and combing regulatory authorities for any information on sanctions against providers.
The company estimates that it reduced associated health plan physician data management costs by 75% through elimination of duplicative work and by improvement in survey execution workflow and other improvements. Sutherland estimates that it reduces the touches on providers from 3 to 1 call per practice, improves reporting and other interactions with the California regulatory body, and improves patient access to timely care.
]]>
NelsonHall recently attended HIMSS19 in Orlando, Florida, the largest healthcare IT conference in the world, with over 45K delegates attending and 1.3K vendors in the exhibition. Here are three highlights from the many conversations we had about the state of the healthcare industry.
Obstacles to improving CX
The conversation about “consumer experience” in healthcare organizations invites harder questions about the challenges and obstacles to building customer intimacy. NelsonHall spoke with leaders at several BPO vendors about CX:
- DXC Technology: Gurmeet Chahal (the new VP & GM - Americas Head for Healthcare & Life Sciences) suggested that the chief obstacle to providing better CX appears to be the governance and supply of better data. DXC observes this is especially true among provider organizations
- Atos: Jack Evans (COO - Digital Health Solutions, North American Operations) suggested that healthcare organizations lack the capacity to effectively manage many constituencies and peer organizations “in a multi-source world” in ways that unite operations in their efforts to promote intimacy with customers across business units and channels
- Genpact: Rakesh Nangia (VP, Life Sciences and Healthcare) suggested that healthcare organizations are stymied in their ambitions because they lack clarity on ownership of CX across the organization. While healthcare organizations are investing and experimenting to improve CX, healthcare organizations have thus far failed to reorganize budgets, people, and technology around CX priorities and measures under comprehensive and authoritative leadership.
Each of these vendors is making significant investments to provide better CX offerings to healthcare industry clients under the rubric of “digital transformation.” DXC has invested in internal data platforms that unite front-office and middle-office functions with security, workflow, and automation capabilities. Atos acquired financial services powerhouse Syntel for $3.4b in July 2018 and aims to make that company’s customer intimacy models relevant and compelling to healthcare clients in North America. Genpact also aims to transplant CX expertise from BFI into the healthcare industry. For more information on Genpact’s September 2017 acquisition of TandemSeven and its relevance to CX, see Rachael Stormonth’s blog here.
RCM in the crosshairs
Many BPO vendors see opportunity in the healthcare provider RCM sector. For background see my blog U.S. RCM Outsourcing Services Market Ripe for Consolidation. BPO vendors often see RCM industry fragmentation and inefficiencies as opportunities for consolidation and automation, and we found this view echoed by major BPO vendors present at HIMSS19. They use similar language to describe enticements and hurdles expanding business in this market segment, remarking on:
- Consolidation in the provider hospital systems market, rationalizing RCM operations
- The large scale of U.S. RCM services market
- Labor arbitrage opportunities for smaller RCM services vendors to move operations offshore
- Automation opportunities for IT-savvy BPO vendors to leverage scalable IT platforms
- The relatively low risk of taking over operations that have limited capital requirements and manage stable cash flows.
Depending on the vantage of the BPO services vendor, the relative immaturity of provider organizations’ procurement functions can be viewed as a positive or as a negative. Incumbent BPO vendors that have cultivated broadly-based, enduring relationships with providers enjoy significant barriers to competition. But those entering the space for the first time similarly must earn trust in complex, decentralized clinical and administrative constituencies (many of which are oriented by mission rather than profit) that prioritize “friends and family.” Several BPO vendors we spoke with appear to be actively exploring opportunities for expanding their businesses, cautiously, in the RCM market segment.
No new news on BPaaS
There was only limited discussion of moving healthcare operations root and branch into outsourcing arrangements. Cognizant has been advocating for healthcare payers of all stripes to focus their strategies and find efficiencies by utilizing its business process as a service contract (BPaaS) offering. The sales cycle for such a deal lasts, we expect, for at least two years, but we aren’t seeing fruit from Cognizant’s efforts.
Furthermore, we didn’t hear new news from NTT DATA. With November’s Q3 financial results NTT DATA announced it had sealed a $200m deal with an as-yet unnamed payer client. The investor presentation had stated that a deal for application management services, BPO, and infrastructure services for a U.S. payer had been signed for a seven-year period with a total contract value of over $700m. However, we have yet to learn additional substantive details.
]]>
The healthcare revenue cycle management (RCM) BPS market is becoming technically more advanced as vendors experiment with RPA to drive greater efficiency and productivity, and to improve competitive positioning. Here I look at one such vendor, Access Healthcare, and the lessons they have learned from their own RPA initiatives.
Access Healthcare generates ~$145m in revenue delivering RCM BPS through 11,000 employees, with operations based mainly in India. Both its President and founder, Shaji Ravi, and its Chairman, Anurag Jain, had worked for Perot Systems’ (and then Dell Services’) healthcare practice prior to Access Healthcare being established in 2010. Access began to make strategic technology investments after Anurag joined in 2012, with the objective of improving productivity significantly beyond what was possible with its India-based labor arbitrage business model.
Lesson 1: Assess whether to build or buy your own RPA platform
Initially, Access Healthcare experimented with various RPA packaged software such as that offered by the leading horizontal vendors. According to Jain, his company discovered that trying to apply RPA packaged software to healthcare RCM processes ultimately proved inefficient. “[Packaged RPA software] is like a big Lego set with no instructions,” he said. “Efficiency with IT assets is the key and we found it more efficient to build our own technology platform.”
Ultimately, the company decided to build RPA capabilities onto the company’s existing IT platform (based on Microsoft.NET and SQL Server), calling the platform arc.in.
Lesson 2: Broaden your perspective when identifying efficiencies from RPA
Experimentation with RPA prompted Access Healthcare to think more broadly about the efficiency of its internal IT function and other areas of its organization, including HR management, data management, and workflow. The company resolved to integrate these considerations into the development of its enterprise platform to simultaneously streamline the management of people, data, and finally, customer-facing RCM processes.
As Access Healthcare worked to move beyond labor arbitrage and a transactional business model, Chairman Anurag Jain said he realized that “the real objective is not to make the customer’s processes and transactions more efficient but instead to make their work disappear.” The implication, he continued, is that it requires deeper partnerships with clients that incentivize all parties to generate and share the benefits from the work that disappears.
Lesson 3: An effective, scalable technology platform can generate M&A and partnership opportunities
An RCM BPS company with an efficient and scalable technology platform can expect to benefit by extending its technology capabilities across the operational functions of other RCM BPS companies and across other RCM market segments. And this can create opportunities for acquisitions of, or partnerships with, other RCM BPS companies.
Jain has pursued this line of thinking as he considers what he believes to be his firm’s cost advantage over other, less technologically advanced, RCM BPS vendors. He groups these cost advantages into two categories: workforce management and automation/analytics.
Workforce management
Access estimates that this category generates a 7-10% operational cost advantage over competitors. The costs of Access Healthcare employees equal those of management, which together far outweigh all other costs. Hence, technology that reduces management and employee costs is prioritized for investment. Access has developed proprietary technology for:
- Workflow tools: data and tasks from 150 payers and 300k+ providers are routed to appropriate teams and individuals, resulting in greater per-seat productivity
- Performance analytics: monitoring systems predict when employees are likely to be dissatisfied, when management intervention is necessary, and how managers can address dissatisfaction
- Automated incentive program: employees are motivated and monitored through use of a reward program that can equate to 20% increase in salary and accelerate promotions
- HR systems: help automatically manage a 2% per month attrition rate while simultaneously growing headcount. Every month, Access uses its software tools to manage 4k candidate assessments and 2k people in the recruitment process.
Automation/analytics
Access estimates that this category generates an 18-23% operational cost advantage over competitors. It estimates that when a bot is successfully deployed, a CSR can be spared 30-40% of his or her effort in executing a given process. After experimenting with tools from UiPath, and having evaluated Blue Prism and Automation Anywhere, Access discovered that it gets better results from its proprietary “echo” RPA software suite developed on its in-house arc.in platform. And because the platform is developed on Microsoft.NET using SQL Server databases, it is relatively easy to find the talent necessary to build and maintain its systems. Points of note here include:
- Process improvement team: The Six Sigma team operates with a holistic view of enterprise and client processes. This team identifies/prioritizes/writes requirements for automation opportunities
- 100+ developer team: This team builds and maintains the proprietary platform and tools, and includes 40+ developers to configure and deploy the proprietary “echo” RPA software suite
- Modular architecture: The company believes that the automation architecture should be built with process components in mind. Micro-bots should be able to automatically hand off work to each other if necessary, and micro-bots added to a library by process SMEs should make the architecture scalable
- Bots: The flexible platform enables a 4-6 week build and deploy period for new bots, and 1k+ bots are in production. Automatic logs enable measurement of the impact of bots on transactions and clients
- ML: Machine learning tools predict payer responses to specific transactions over time, enabling Access Healthcare to define and customize more effective workflows. ML tools also help prioritize investment in building and deploying new bots
- Point solutions: The company has also created platform-compatible applications for payment posting, claims follow-up, and denial management.
Confident in the advantages conferred by its own technology platform, Access Healthcare acquired Pacific BPO, another RCM BPS company in an adjacent healthcare market segment, in September 2018. Having assessed that company’s functional processes to be largely manual, Access believes it can use its platform to generate significant efficiencies. Access also believes that it can bring a new level of technology sophistication to a market segment ripe for the introduction of process re-engineering and automation.
]]>
The challenge of rising healthcare costs in the U.S. has been obvious for decades. Or has it? Various interventions have been attempted, but health costs as a percentage of GDP are forecast to continue to climb. National U.S. healthcare expenditure as a percentage of GDP has risen from 17.2% in 2011 to 17.9% in 2017.
In February 2018, the U.S. CMS Office of the Actuary estimated that “growth in national health spending is projected to be faster than projected growth in GDP by 1.0 percentage point over 2017-2026. As a result, the report projects the health share of GDP to rise from 17.9 percent in 2016 to 19.7 percent by 2026.” GDP growth over the last two periods has kept pace with rising healthcare costs over the last two years, but when GDP growth subsides, the healthcare cost challenge will reemerge. The current stalemate at the U.S. federal level about the path forward for healthcare reflects a lack of consensus about root causes and, therefore, advisable policy.
The sector has already undergone major restructuring and intervention, both government and private sector initiatives. This includes:
- The American Recovery and Reinvestment Act of 2009 (ARRA) incentivized adoption of EHRs – the assumption was that a lack of electronic clinical records technology was a primary component of inefficiency and waste. 90%+ of U.S. hospitals have now adopted EHR technology
- The Accountable Care Act (ACA) of 2010 realigned much of American healthcare reimbursement and delivery – the assumption was that decentralized, misaligned organizations created waste and reduced quality. The ACA introduced a raft of initiatives designed to address waste and improve productivity, particularly clinical labor productivity. The results of most of these measures, including the ACA’s Accountable Care Organization initiatives (ACOs) remain inconclusive
- Consolidation: the payer and provider markets have been roiled by restructuring and consolidation. There were 1,412 hospital mergers between 1998 and 2015; physicians also have consolidated into increasingly larger groups. Moreover, the four largest insurers now account for 83 % of the total national market.” [1].
The largest target for improvement in healthcare delivery costs remains the cost of labor. But does more “technology” improve labor productivity? Not necessarily. Technology can drive rather than retard growth in healthcare costs. According to a Health Affairs (HA) article, “technological changes in the [physician and nursing] sector to date have favored, rather than substituted for, those with high skills" [2]. It depends on the type of work or process, on the technology use case, and on the organizational aptitude for adopting new solutions. Administration, management and IT are oft-cited as a source of burgeoning healthcare delivery costs, but these classes of labor may actually be seen as examples to be followed. Over the 15-year period of the HA study, compensation (change in employment x change in earnings) for administration, management and IT rose only 35.3%. Over the same period, compensation for physicians and nurses rose 80.5%.
Taking a step back, have all the industry-level efforts at restructuring mentioned above missed the mark? Have we simply failed to appreciate how unhealthy Americans have become – and therefore overlooked the root cause of precipitous cost increases? The debates and struggles regarding GDP growth, healthcare delivery cost growth, technology adoption, government intervention, and market restructuring may simply be addressing symptoms rather than causes of the rise in U.S. healthcare costs.
The “hidden in plain sight” fact may be that Americans have unhealthy habits which have national ramifications for healthcare costs. In one 2013 study, only 2.7% of the U.S. adult population could be identified with healthy metrics for exercise, diet, smoking, and body fat. As national healthcare expenditures rise towards 20% of GDP, perhaps we should ask whether the challenge of rising healthcare costs can be adequately addressed by industry-level restructuring efforts. Perhaps this challenge can better be addressed by bottom-up rather than top-down initiatives.
[1] The Commonwealth Fund, Insurer Market Power Lowers Prices in Numerous Concentrated Provider Markets, September 6, 2017
[2] Where the Money Goes: The Evolving Expenses of the US Healthcare System, Health Affairs, July 2016

In 2016, Atos was awarded a 13-year life & pensions BPO contract by Aegon, taking over from the incumbent Serco and involving the transfer of ~300 people in a center in Lytham St Annes.
The services provided by Atos within this contract include managing end-to-end operations, from initial underwriting through to claims processing, for Aegon's individual protection offering, which comprises life assurance, critical illness, disability, and income protection products (and for which Aegon has 500k customers).
Alongside this deal, Aegon was separately evaluating the options for its closed book life & pensions activity and subsequently went to market to outsource its U.K. closed book business covering 1.4m customers across a range of group and individual policy types. The result was an additional 15-year deal with Atos, signed recently.
Three elements were important factors in the award of this new contract to Atos:
- Transfer of the existing Aegon personnel
- Ability to replatform the policies
- Implementation of customer-centric operational excellence.
Leveraging Edinburgh-Based Delivery to Offer Onshore L&P BPS Service
The transfer of the existing Aegon personnel and maintaining their presence in Edinburgh was of high importance to Aegon, the union, and the Scottish government. The circa 800 transferred personnel will continue to be housed at the existing site when transfer takes place in summer 2019, with Atos sub-leasing part of Aegon’s premises. This is possible for Atos since it is the company’s first life closed block contract and the company is looking to win additional deals in this space over the next few years (and will be going to market with an onshore rather than offshore-based proposition).
Partnering with Sapiens to Offer Platform-Based Service
While (unlike some other providers of L&P BPS services) Atos does not own its own life platform, the company does recognize that platform-based services are the future of closed book L&P BPS. Accordingly, the company has partnered with Sapiens, and the Sapiens insurance platform will be used as a common platform and integrated with Pega BPM across both Aegon’s protection and closed book policies.
Atos has undertaken to transfer all of the closed block policies from Aegon’s two existing insurance platforms to Sapiens, and these will be transferred over the 24-month period following service transfer. The new Sapiens-based system will be hosted and maintained by Atos.
Aiming for Customer-Centric Operational Excellence
The third consideration is a commitment by Atos to implement customer-centric operational excellence. While Aegon had already begun to measure customer NPS and assess ways of improving the service, Atos has now begun to employ further the customer journey mapping techniques deployed in its Lytham center to identify customer effort and pain points. Use of the Sapiens platform will enable customer self-service and omni-channel service, while this and further automation will be used to facilitate the role of the agent and enhance the number of policies handled per FTE.
The contract is priced using the fairly traditional pricing mechanisms of a transition and conversion charge (£130m over a 3-year period) followed by a price per policy, with Atos aiming for efficiency savings of up to £30m per annum across the policy book.
Atos perceives that this service will become the foundation for a growing closed block L&P BPS business, with Atos challenging the incumbents such as TCS Diligenta, Capita, and HCL. Edinburgh will become Atos’ center of excellence for closed book L&P BPS, with Atos looking to differentiate from existing service providers by offering an onshore-based alternative with the digital platform and infrastructure developed as part of the Aegon relationship, offered on a multi-client basis. Accordingly, Atos will be increasingly targeting life & pensions companies, both first-time outsourcers and those with contracts coming up for renewal, as it seeks to build its U.K. closed book L&P BPS business.
]]>
The healthcare revenue cycle management (RCM) outsourcing services market in the U.S. seems ripe for disruption and consolidation. The macro factors include:
- Contraction in the number of hospital locations and hospital systems
- Speedy erosion in the number of small, independent physicians’ practices
- Increasing complexity in reimbursement models and processes
- Increasing experience and scale of off-shore service vendors
- Decreasing costs of managing RCM operations RPA followed by broader AI and digitalization technologies.
The landscape of RCM platform and outsourcing vendors is highly fragmented and provider organizations considering outsourcing have numerous options. Becker’s Hospital Review listed 110 software and/or services vendors in this space in 2016 and expanded that list to over 160 vendors in October, 2017. Will the RCM outsourcing market become the target of a well-capitalized player or set of players, and if so, will technology be a primary driver of RCM industry consolidation?
Some vendors in the RCM industry certainly appear to have advanced down this line of thinking. Recently I spoke with Anurag Jain, Chairman of Access Healthcare, an India-based RCM BPS vendor, about the disruption and consolidation that he and his company anticipate. Jain believes that if the appropriate automation can be overlaid on standardized, optimized processes and people management systems, then the opportunity to take cost out of U.S. RCM far outstrips the capacity of his own company (and, he implied, the capacity of many of his competitors) to meet that opportunity through organic growth. As a result of this opportunity, Jain foresees a major capital infusion into the U.S. RCM outsourcing industry, with consolidation being one of the consequences.
Jain is excited about this prospect because he believes his company has the people, process, and technology capabilities to create a platform for such consolidation. Regarding Jain’s own company, privately held Access Healthcare recently announced that it had acquired privately-held Pacific BPO. According to Jain, as of August 31, 2018, operations of the combined entity will mobilize over 11,000 employees and 19 delivery centers in the U.S., India and the Philippines to serve over 70 customers, with the combined entity now commanding estimated revenues of $140m.
Another indication that an acceleration of industry-wide consolidation is in the air is the news that UnitedHealth is one of a number of companies looking to acquire Tenet’s Conifer business. What if Conifer is indeed acquired by UnitedHealthcare Group, and then grafted onto its subsidiary, Optum? Conifer manages $1.6bn in RCM outsourcing revenue with about 14,000 employees. Overall, Optum revenues are $91bn, and Optum’s RCM business employs 7,700 people. The scale and potential efficiencies of a combined Conifer/Optum RCM business could precipitate further consolidation. The fact that United (and Optum) are interested in acquiring Conifer indicates that Tenet, CHI, and United all see opportunity in consolidating the U.S. RCM outsourcing market, and this indicates that Access Healthcare may be one of the pioneers in a broader industry restructuring.
]]>
NelsonHall recently attended the SE2 Partnership Forum, entitled ‘Future-proof: From Here to Digital’, in Washington D.C., where the main focal point of discussion was the challenge of digital transformation in the life insurance and annuity sector.
Here I look at a number of developments in SE2’s offerings that are helping clients to address the challenge of digital transformation.
Digital consumer experience
SE2 offers multi-channel consumer engagement, deploying chatbots (or ‘roboadvisors’) to optimize the customer experience, including an interactive messenger with cognitive capability. It also uses machine learning and analytics.
SE2 uses Alexa to provide self-service capabilities, whereby customers can use voice activation to request policy details, change premium schedules, and receive dedicated virtual assistance and offers on new products and plans. As well as increasing personalization and improving the customer experience, this also increases cross-sell and upsell opportunities.
For digital content delivery, SE2 uses Broadridge, which encompasses three areas:
- Experience management: replacing static documents and emails with dynamic, personalized and relevant digital communications
- Omni-channel communications: delivered to traditional electronic channels (email/SMS) and to personalized cloud solutions and online banking interfaces
- Data and analytics: offering improved digital adoption, enabling customers to set digital preferences.
SE2’s digital content delivery improves the customer experience, helps reinforce value propositions and promote new products, and goes beyond email with new digital channels. It allows clients to select preferred communication channels, offers a network of insurance brands that help drive digital adoption, and enables continuous improvement via robust analytics.
Digital Direct Life platform
The Digital Direct Life platform provides an enhanced, responsive UX and includes configurable eApp, Questions for D2C, and Agent Assisted Apps. Its Open Integration Architecture with OOB connectivity to major third-party providers includes vendors used for gathering evidence in life underwriting (MIB, MVR, Rx, etc.) and medical vendors (Lab, APS, etc.). It has a notification center with continuous multi-channel updates that enables self-service and integration with UW platforms using industry standards (ACORD) for automated and manual UW connected to a multi-channel payment gateway.
The platform uses Automated Underwriting (AU) with Electronic Health Records (EHR), with advanced techniques like Application Triage Algorithms, to achieve automated application decisions without any manual review in 75% of cases. This reduces underwriting time from the current 30-45 days to near immediate delivery, with the cost reduced from $400 to less than $50.
AU with EHR provides a single point for collection, consolidation, text mining, and reporting of EHR data, helps distribution channels close leads faster, helps insurers improve customer experience, increases revenues, and reduces cost. It also makes health and wealth management seamless, bypassing invasive underwriting procedures involving lab work (e.g. blood testing).
Improving speed to market
SE2 has applied the following technology enhancements to enable clients to improve their speed to market:
- A template-driven responsive website offers optimized web experience. Self-service administration toolsets are presented on a responsive web design pattern that is device agnostic and comes with a notification center
- Digital integration platform, which provides client-centric business services delivered with a scalable business integration architecture. The open architecture leverages industry standards across internal and external partner ecosystems, leveraging Mulesoft, ActiveMQ, and Informatica
- Enterprise output framework, a real-time framework enabled for scheduled transactions, with consistent template management utilizing the carrier’s branding. Its Output Manager manages on-premise and offsite print and mail capability, and also provides enhanced audit and compliance across the print and delivery lifecycle, along with integration with partner channels like Broadridge for e-delivery
- An actuary engine (from Accenture) provides a configuration-driven product rule engine that allows granular configuration of transactions and scheduled events. A modern UI controlled by a security layer and seamless integration with the SE2 annuity Policy Administration System (PAS) reduces the effort to implement product rule changes.
Future proofing initiatives
SE2 is also involved in a number of initiatives with the aim of providing ‘future-proof’ life & annuities capabilities for its clients, including:
- Blockchain. SE2 is on the LIMRA Blockchain Advisory Board, and indicates that there is a consensus among carriers on the positive impact of Blockchain, evaluating technologies and conducting POCs that require industry-wide collaboration. Leveraging learnings from other industries, including P&C insurance, and identifying potential use cases for industry-wide solutions helps improve peer-to-peer settlement in Blockchains. Benefits are derived in the form of increased transparency, accurate tracking, permanent ledger, and cost reduction
- Virtual and augmented reality that enhances the user experience with richer content, provides real-time information enmeshing of real and virtual worlds, training and advocacy to increase effectiveness and efficiency, and design visualization for heightened experience and insights
- Insight-driven analytics (from DataRobot). Along with its partners, SE2 is helping its clients achieve state-of-the-art in life underwriting by combining the power of predictive analytics with the SE2 platform. Insights derived from the SE2 platform are augmented with third-party data (e.g. from MIB, MVR, Rx, and APS) to create an analytics partner ecosystem operating as a one-stop shop, with annuity and life analytics driving decisioning, and advanced technology using a data lake and machine learning.
Summary
The global life insurance market is being transformed rapidly due to the increased adoption of digital solutions, providing opportunities for life companies to gain competitive advantage by responding quickly to changing market forces, consumer needs and preferences.
SE2’s deep domain experience and commitment to digital transformation are key strengths in this market. The company backs its own investments by partnering with startups to reduce speed to market and provide greater efficiencies. SE2’s strategy to develop world-class digital life insurance solutions recognizes the power of both innovation and collaboration in realizing this goal.
]]>
NelsonHall recently caught up with Genpact to discuss their recent acquisition of OnSource and their plans to integrate it with BrightClaim – we were not surprised to hear that the two acquisitions are indeed connected, and part of Genpact’s strategy to introduce new digital process models in P&C insurance.
To set the scene:
- Earlier this month, on the day of its Q2 earnings results, Genpact announced it had acquired OnSource, a small software house based in Boston, MA. On its own, OnSource will not make a meaningful contribution to revenues
- In May, Genpact announced it had acquired BrightClaim, a U.S. domestic P&C insurance BPS provider with centers in Atlanta, GA and Austin, TX and its associated company National Vendor that provides content evaluations, through its large field force, and content fulfilment services.
Genpact has an active M&A strategy currently; the priorities include adding
- Digital and analytics capabilities to help accelerate the build out and deployment of digital assets, as OnSource does
- Domain capabilities in targeted verticals and services, as BrightClaim does.
BrightClaim brings in a new client base of Tier 2 carriers for Genpact to cross-sell its services - and indeed the short-term opportunities include adding global delivery options for some of its services offerings. But the strategic opportunities are in applying disruptive technologies to some of the touchpoints and currently manual interventions within the claims process. And OnSource provides an opportunity to do this in certain areas.
Applying digital solutions from auto FNOL to improve the inspection and appraisal processes in property claims
Now BrightClaim’s client base is around 85% property/15% auto insurance, whereas OnSource has essentially the reverse ratio with its client base - so what are Genpact’s plans in integrating these two companies, based in different regions, and serving different segments?
Quite simply, they center on applying Onsource’s ‘Inspection-as-a-Service’ solution, developed initially for the auto insurance market, to the loss estimating process in property claims. The solution uses either mobile devices or drones to obtain photos and videos (also written evidence) that are used to assess damage and generate loss estimates for claims payouts. Carriers can use the solution to offer customers, when making a claim, a choice of:
- A self-service approach to the FNOL process, using the OnSource ‘Instant Inspection’ mobile app to connect to a Virtual Appraiser’s desktop for a claim submission. The photographic evidence provided can be downloaded directly to the insurer’s appraisal software. The app can also be used by motor repair shops for any supplement approvals
- An assisted solution using a network of 17k ‘Uber-like’ field photo inspectors who can walk the customer through the claim submission process using an iPad.
The benefits of Onsource’s ‘Inspection-as-a-Service’ solution for carriers and also their customers are obvious:
- In terms of the customer experience, either method (self-service or assisted) offers ease of use and a significant reduction on the traditional cycle time – Genpact claims by around 30%
- And for the carrier, there are major cost reductions in loss adjustment expenses (LAE) from eliminating the traditional field inspection process and from more efficient workflows - Genpact claims by 50% plus – and the visual MOI can also mean more accurate indemnity.
In short, digitizaling this process can help in improving three priorities which carriers have to balance: customer satisfaction, expense control and loss control.
The use of mobiles in submitting photographic and video evidence of damage in auto claims is now very well established, and the use of drones as a Method of Inspection (MOI) for high value/ hard to access property claims assessments has also been gaining traction in many Tier 1 carriers over the past few years – but both methods remain fairly new for Tier 2 carriers in their personal property lines. Video technology will become increasingly important across the P&C insurance sector over the next few years. The FAA has taken some time in sorting out regulations for the commercial use of drones which slowed things down slightly: OnSource brings with it a nationwide network of certified drone operators; this capability has the potential to transform the independent property appraisal services offered by BrightClaim. The ‘Instant Inspection’ app could also be applied to some of the contents evaluation services provided by National Vendor, enabling some activities to be done remotely.
Genpact’s integration streams for OnSource and BrightClaim are moving at pace.
With its P&C BPS services, Genpact has positioned on its domain knowledge combined with expertise in lean process mapping, intelligent automation, and workflows for straight-through processing, analytics, as well as offshore delivery. With OnSource, Genpact has another digital solution it can offer to BrightClaim’s carrier client base.
Further Acquisition Activity in Support of New Digital Process Models by Genpact Highly Likely
Genpact is one of a number of BPS specialists that have in the last few years been energetically reinventing their portfolios to embrace the sometimes dramatic shifts afforded by Digital in enterprise operations and develop new digital business process models (NDPMs).
Genpact’s other acquisition this year was that of Rage Frameworks, whose NLG software has enhanced its AI capabilities. We expect to see more investments by Genpact soon, including possibly acquisitions that bring more cognitive tools into the Cora platform, and/or more consulting-rich domain expertise to help clients in the digital transformation of their middle and back offices.
]]>
Genpact has had a traditional presence in offshore-based adjudication support services for the property & casualty sector but is now, supported by its acquisition of BrightClaim, aiming to reposition as a disruptive provider of claims managed services.
The acquisition of BrightClaim provides Genpact with deep onshore domain and loss adjusting capability, which Genpact is looking to combine with its offshore services and a new digital operating model to enhance its value proposition to P&C firms.
In particular, Genpact is looking to extend its value proposition beyond the traditional BPO proposition of expense control to impact both loss control and customer satisfaction. Its new value proposition for low-medium complexity claims across property and auto encompasses:
- Claims operations cost reduction of up to 40%
- Improving customer experience, CSAT, and NPS by 10%-20%
- Reducing the cost of losses by 3%-5%.
Introducing a New Digital Process Model for Claims
While most carriers have introduced apps and self-service at the front-end, and use of photos has become commonplace in auto claims, Genpact perceives that there has so far been a much lower level of innovation in property claims processes and is aiming to take advantage of this lack of delivery maturity. Genpact has accordingly established a new digital business model that encompasses end-to-end claims services across both property & auto claims. It includes:
- FNOL & claim set-up: using digital channels, IoT and smart home sensors, Intelligent Automation for claim set-up & verification, analytics & Big Data for claims triaging, fraud and subro identification
- Loss estimating: use of photos and drones and computer vision to enhance turnaround time and improve customer service, and integration of estimating tools with claims systems
- Adjudication: automation of fraud, subro and litigation propensity using analytics & Big Data; and using Intelligent Automation in support of claims verification, updating, and communication
- Special Investigation Unit & Litigation Management: supported by Big Data and analytics
- Payment, recovery & claim closure.
BrightClaim: Complementing Genpact’s Offshore Services with Onshore Desk and Field Assessors
Earlier this month Genpact acquired BrightClaim, a P&C claims administrator company based out of Atlanta founded by ex-Crawford executives. BrightClaim and its associated company National Vendor have full P&C policy lifecycle claims and administration capabilities for low and medium complexity claims, including an extensive network of contractors. BrightClaim segments its business into:
- Property field services
- Catastrophe
- Contents services (through BrightClaim’s 2016 acquisition of National Vendor)
- Liability/auto
- Warranty (now viewed as non-strategic)
- BrightServ (managed repair program through its network of contractors, includes a partnership with Home Depot).
BrightClaim has around 200 employees in Atlanta and Austin conducting desk reviews and estimation and managing BrightClaim’s network of ~1,000 field property adjustors. These field loss adjustors could also be used as a desk appraisal resource as Genpact increasingly replaces physical onsite reviews with photos from mobiles sent by the customer and drone images, the latter being particularly applicable for property roofing assessments. Genpact intends to incorporate drone services into its delivery and has several drone pilots underway with carriers. The fact that BrightClaim’s field loss adjustors are contractors rather than employees made the acquisition particularly attractive as it facilitates the drives towards an increasingly digitized service delivery model.
BrightClaim has its own loss adjusting systems which connect to core insurance systems such as Guidewire and legacy P&C platforms and to the principal estimating platforms used in the U.S. Genpact will create a common platform around these using PNMSoft for workflow and incorporating automation and cognitive technologies to achieve its new digital business process model around claims.
Extending Targeting to Mid-Tier P&C Carriers
BrightClaim has around 100 P&C carrier clients, including half of the top 20 U.S. carriers, and there is some overlap with Genpact’s existing U.S. P&C client base. Its focus is on low to medium complexity claims which can be more readily digitalized, with a 70/30 mix between personal and commercial. In the property space, Genpact will target personal and light commercial claims, while all auto third-party liability activity is in support of personal claims.
Genpact’s priority is the top-tier P&C firms where it is looking to sell three broad groups of services while demonstrating synergies and digital integration between these:
- FNOL & claims triage, likely to be a growing area of activity with Genpact promoting how analytics can drive value downstream in the claims value chain
- Loss adjusting and claims adjudication, using blended onshore/offshore delivery
- Subrogation, fraud, and recovery services.
In addition to targeting top-tier carriers for transformation of parts of the value chain, the BrightClaim acquisition also creates an opportunity for Genpact to target mid-tier U.S. P&C carriers with end-to-end claims services supporting them in the digital transformation of their entire value chain. Several conversations of this type are already underway.
Genpact has been on a bit of an acquisition spree recently, and this is not likely to pause. BrightClaim is a U.S. operation, and Genpact is looking for a similar opportunity around claims management services in the U.K., Germany or the Netherlands – expect to see another regional claims-related acquisition.
]]>
On March 15, WNS announced its intended acquisition of HealthHelp, in what, at $95m, will be its largest acquisition to date. HealthHelp, founded in 1999 and headquartered in Houston, TX is a 400-FTE strong healthcare utilization management specialist.
In many ways, the HealthHelp acquisition has much in common with WNS’ Value Edge acquisition. HealthHelp, like Value Edge, will become part of WNS’ healthcare business unit and is rooted in research & analytics. While WNS’ healthcare unit has a traditional “administrative” BPS business, around claims, billing, & collections, serving healthcare payers, the bulk of WNS’ healthcare revenues are derived from the pharmaceuticals sector. This acquisition is intended to assist WNS’ healthcare unit in achieving a more balanced revenue mix between healthcare payer and pharmaceuticals.
Targeting Direct Care Costs in Addition to Administrative Costs
The acquisition gives WNS’ healthcare payer capability a major boost and enables WNS to position on reducing the direct cost of care for healthcare payers, and not just on reducing their administrative costs. Post-acquisition, WNS is now going to market in the healthcare payer sector with a combination of administrative BPS services, analytics, and the collaborative care management services from HealthHelp. WNS was already targeting its existing healthcare payer BPS clients with analytics services, though mostly on a project basis; this acquisition provides it with an opportunity to enhance its existing healthcare analytics capability with a high value-add service to assist payers in establishing improved treatment rules and guidelines in collaboration with providers. WNS is already in conversation with several large national payors regarding its new combined offering and will be targeting both national payors and regional payors.
And, of course, in addition to targeting existing WNS healthcare payer clients and prospects with its HealthHelp capabilities, WNS will target existing HealthHelp clients with its complementary established claims management and analytics capabilities.
Cross-Fertilizing into Workers’ Compensation
Because of the complementary nature of HealthHelp’s services and WNS’ existing healthcare payer offerings, the integration of HealthHelp into WNS should be relatively straightforward leaving the delivery organizations of the existing entities largely unchanged. The principal integration activities involve creating a joint go-to-market and integrating WNS’ existing technology with HealthHelp’s Consult software.
In addition, WNS has evaluated using HealthHelp’s Consult pre-authorization tool in support of workers’ compensation utilization, which uses similar data sets to healthcare payer, and pharmaceuticals utilization, and is likely to enhance Consult to support workers’ compensation in the near future.
Supporting an Under-Penetrated Market
HealthHelp began life supporting Humana and was initially centered on supporting Medicaid and Medicare claims. Indeed, Humana still accounts for over 60% of HealthHelp’s revenues; it now also has contracts with a number of smaller payors. So WNS and HealthHelp have an under-penetrated market with considerable potential opportunity.
The areas currently supported by HealthHelp’s collaborative care management are cardiology, radiology, oncology, pain & orthopaedic, sleep care, and emergency medicine. For each of these areas, HealthHelp has established “evidence-based guidelines to directly help providers order the most appropriate tests and procedures for their patients”. The service works on a non-denial basis and aims to reduce the cost of treatment to payers by educating providers on the most appropriate procedures and avoid unnecessary or inappropriate tests and treatment.
This knowledge is encoded in HealthHelp’s Consult clinical decision support platform which provides healthcare providers with guidance for performing the most appropriate tests and procedures and typically approves 75% of provider recommendations automatically, with the remaining 25% being subject to HealthHelp’s nurse review. Here, HealthHelp nurses collaborate with physicians to discuss alternative treatments and propose clinical guidelines more relevant to the patient’s condition. HealthHelp has ~400 FTEs with the majority based onshore in the U.S. principally in Houston. Other U.S. locations include a contact center in Albany, New York, and an office in Annapolis, Maryland from where it serves the radiology community. In addition, HealthHelp has customer service personnel based in the Philippines. The company also collaborates with ~100 MDs and 11 university medical systems, that are involved in guidance in ~6% of more challenging cases, with HealthHelp supporting the physician seeking guidance with a specialist in their field.
HealthHelp estimates that removing the threat of denial and providing “collaborative consultation and education between providers and payors’ utilization management organizations” has resulted, for example, in 15%-30% savings for radiation oncology and 12%-25% for medical oncology.
At the same time, HealthHelp’s utilization management process aims to reduce the overuse of screening and diagnostic tests by detecting redundant testing, sequential testing, and physicians billing for unauthorized procedures.
A further benefit to payers is that many of HealthHelp’s services qualify as “activities that improve healthcare quality” within the MLR requirement and so do not count as an administrative cost to payer organizations.
Pricing for HealthHelp is currently based on a standard PMPM (per member per month) model. WNS may look to evolve this to outcome-based pricing models as it looks to assist healthcare payers in driving down the overall cost of medical care.
Opening the Door to Regional Payers and Healthcare Systems Outside the U.S.
In summary, the acquisition of HealthHelp lifts WNS’ healthcare payer proposition beyond the legacy and mature area of administrative cost reduction into direct care cost reduction and provides WNS with an onshore “door-opener” for both national payors who have traditionally been receptive to offshore-centric administrative services and for regional payors, who have not.
The new capability also potentially has applicability to other areas of the wider healthcare-related industry where organizations need to reduce direct treatment costs, including workers’ compensation, pharmaceutical spend, and even potentially healthcare systems outside the U.S. Here, WNS could potentially target the NHS in the U.K., a country where WNS has an existing strong presence.
]]>NIIT Technologies has a clear focus on a few target industries, with Travel & Transportation accounting for nearly a third of its global revenues, Insurance nearly 25% and Banking & Financial Services another 20%. From a service line perspective, ADM represents the bulk of activity (around two thirds of global revenues) and infrastructure management services another 17%.
An emphasis of the half-day event was how NIIT Technologies is moving away from its traditional model, one that was essentially ‘lift and shift’ with expertise and software IP in a few select sectors, to be one that is more clearly focused on customer satisfaction and digital outcomes
CEO Arvind Thakur outlined three strategic priorities for the company:
- 'Smart IT’ (automation/AI)
- Superior Experience
- Scale Digital
Smart IT: Enter TRON
Not the 1982 original, nor the 2010 sequel (both starring Jeff Bridges) TRON is the moniker that NIIT Technologies has recently given to its growing portfolio of smart automation tools for use across infrastructure, applications and business process services. It has partnerships with the likes of UiPath for BPO and with Nanoheal for its IT helpdesk operations. Expect to hear more partnership announcements and additions to TRON.
Superior Experience: Hi 5 for a millennial workforce
Thakur reminded us how NIIT Technologies has sought for some time to engender an organizational culture of “Up Your Service”, with its ‘Hi 5’ approach.

Hi-5
Geared toward a younger workforce, and explicitly encouraging employees to be customer-centric, to question everything and have the confidence to unleash new ideas, we imagine Thakur’s personal pleasure whenever a young employee approaches him with a high five.
Current initiatives include widespread training on design thinking and building design studios. Again, expect to hear more about the latter.
Scale Digital
NIIT Technologies has joined the rank of service providers who are revealing what proportion of their revenues come from “digital services” (though none specify what these cover). In its most recent (Oct-Dec 2016) quarter, management claims that digital services accounted for 19% of its total revenue, up from 15% in the prior year quarter. More important than the percentage itself is the level of topline growth this indicates: by our estimates, this represents a y/y growth of nearly 30% from “digital services”. For a company whose overall topline grew by just 2% last quarter, ‘Scale Digital” is clearly a priority.
New Global Head of Digital Services
The importance of the Scale Digital strategic pillar is reflected in the decision, rather than to replace the COO position, to instead to create a new EVP role of Head of Digital Services, and appointed in January Joel Lindsey (ex. HPE digital transformation program lead). It is still early days; we will be looking with interest to see where and how he chooses to focus.
Digital Experience
NIIT Technologies’ clients are primarily in B2C sectors (T&T, BFSI, media), where digital transformation strategies have centered around the customer experience. Accordingly, NIIT Technologies articulates its approach with digital uses a deep understanding of customers’ pain points and moments of truth to help clients develop sector-specific ‘Digital E3’ (Emotionally Empathetic Experiences):
- Travel and transport, being made to "feel special"
- Investment banking, "feeling secure"
- Insurance, "feeling cared for".
Digital Analytics
We also heard briefly about ‘Digital Foresight’, a proprietary framework and platform which integrates internal company data, external public data (from commercial sources and from social media), and applies predictive analytics. The focus is on BFS and transportation sectors, and organizations handling large volumes of transactions. See an earlier blog about Digital Foresight here. Again, we expect to hear more about ‘Digital Foresight’ and its application in other sectors.
Platforms: new head of NITL
Another element of NIIT Technologies’ positioning on its abilities to support clients on their digital transformation journeys is its platforms business, in particular, its London market software arm NIIT Insurance Technologies Ltd (NITL). Examples of investments in recent years include the Navigator, Acumen and Exact components for multi-market analytics and risk aggregation, and the Advantage multi-market microservices platform, which also supports technologies such as IoT.
The NITL business is not a major revenue generator in itself and growth is currently flat (a consequence of Brexit), but it is a high margin (~20%) business that provides NIIT Technologies with a clear presence in the London Market.
And, again, there is a recent EVP-level hire to head NITL: Adrian Morgan (formerly at London Market competitor Xchanging where he established Xuber, then at CSC where he was also UK Head of Digital for Insurance). His appointment indicates the importance being attached to growing NITL (which has had around $25m investment in platform development in recent years) – perhaps Morgan will try to take Advantage into other regions such as Singapore? Certainly, we should expect to hear more about NIIT Technologies platforms business.
NIIT Technologies has had several quarters of low single-digit growth, impacted most recently by short-term headwinds such as a client-specific weakness in the U.S. travel sector and by an Indian government sector contract, also by current uncertainties in the London market due to Brexit. A return to double digit growth is not likely on the next couple of quarters.
However, there is a very evident emphasis from the top on driving automation and on shifting its business to digital services and to growing the platforms business. In these regards, NIIT Technologies is holding its own with much larger IT services players. The company also benefits from its strong focus on a few target sectors, in several of which it has a significant presence.
The EVP-level appointments of Joel Lindsay and Adrian Morgan (and the naming of TRON!) are clear indicators of investment priorities. We expect to see some interesting announcements coming out of NIIT Technologies in the next few years.
Mike Smart and Rachael Stormonth
]]>
The insurance outsourcing industry is moving at a fast pace in response to the need for rapid deployment of digital platforms and offerings, as well as advancements in new distribution models that are emerging via ‘insurtech’ start-ups. Here I take a look at some of the key trends driving the insurance BPS market in 2017, both in terms of delivery and transformation, and by individual service line.
New distribution models, analytics & automation
Health insurance start-ups (Oscar Health, Clover Health, Bright Health, etc.) have been flourishing, followed by property & casualty insurance (Lemonade, Verifly, Metromile, Wrisk, etc.) and life & annuities insurance (Ladder, League, InforcePro, etc.), who are also seeing an increasing amount of investment. Outsourcing vendors will be actively looking to partner with, or potentially acquire, such companies in order to leverage their capabilities on an add-on basis, or using a completely transformative approach. And the insurance start-ups that will be most targeted by vendors are those investing in new distribution models.
Insurtech developments will bring more regulations at federal level in the U.S., as the application of new operational models will overtake the current state-level regulation framework of insurance companies. It is also possible that the new regulations will allow for the fostering of further innovation compared to current state regulatory frameworks.
Big data and analytics in insurance will see further growth, stemming from the vast amounts of data stored by insurance carriers. Vendors will either develop offerings to leverage such information, or will acquire companies in order to do so. It is still commonplace to find old-school insurers who are unable to analyze and leverage their clients’ and prospective clients’ data.
In terms of operating systems, vendors will continue to optimize legacy platforms with add-on proprietary or third party software, as well as retire dysfunctional and costly systems for newer ones that have modern distribution model capabilities. Digital transformation will increase among insurers, with larger numbers of insurance carriers shifting their operational model towards emerging market segments (millennials, middle-market consumers, etc.).
In the area of automation, the insurance sector has been at the forefront of RPA adoption to date, and this will continue in 2017. Meanwhile, AI technology is taking small steps towards greater adoption within insurance offerings, mostly in policyholder-facing applications. Policyholders will continue to request better, more personalized, engagement by their carriers through omni-channels, with a digital approach, with the policyholder engagement market segment seeing growth of more than 10% per annum.
Elsewhere, wider application of telematics offerings among passenger vehicles and industrial devices will allow for more accurate and individualized calculation of premiums.
Trends for 2017 by insurance service line
Property & Casualty BPS trends include:
- Launching new digital products and services in untapped markets for traditional insurers
- Emergence of fully digitally-operating carriers with a Bermuda-style regulatory framework, backed by PE/VC firms
- Emergence of new products for traditional insurers (drone insurance, on demand insurance, etc.)
- Wider application of analytics for process improvement and trend identification among policyholders.
Life & Annuity BPS trends include:
- Insurers outsourcing more responsibility to vendors that are able to provide specialized actuarial and predictive analytics services targeting customer retention
- Insurers requiring guidance on regulatory product adjustment from Solvency II implementations
- The middle-income and millennials market in the U.S. will see increased growth, as investments in digital channel communications expand
- Vendors will continue to improve customer service levels, CSAT scores and customer retention rates.
Healthcare Payer BPS trends include:
- The future of Obamacare and health insurance exchanges in the U.S. is uncertain after the Trump election. There will definitely be changes in the ACA care models and payers will most probably bear some of this cost of change in healthcare policy
- Consolidation among lower-tier healthcare payers will continue its momentum in 2017, creating opportunities for legacy platform retirements and updates from outsourcing vendors, eliminating disparate assets in newly-formed organizations
- Population health management and wellness programs through innovative delivery and distribution models will see significant growth, as well as engaging with patients through omni-channels, improving retention and satisfaction
- Applying analytics that identify opportunities for process improvement, as well as reducing fraud, waste, and abuse will be a top priority for payers
- Distant monitoring of patients and telemedicine will also see increased growth
- Preventive care and wellness offerings, in conjunction with traditional healthcare insurance, will see a rise in demand.

As well as conducting extensive research into RPA and AI, NelsonHall is also chairing international conferences on the subject. In July, we chaired SSON’s second RPA in Shared Services Summit in Chicago, and we will also be chairing SSON’s third RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December. In the build-up to the December event we thought we would share some of our insights into rolling out RPA. These topics were the subject of much discussion in Chicago earlier this year and are likely to be the subject of further in-depth discussion in Atlanta (Braselton).
This is the third and final blog in a series presenting key guidelines for organizations embarking on an RPA project, covering project preparation, implementation, support, and management. Here I take a look at the stages of deployment, from pilot development, through design & build, to production, maintenance, and support.
Piloting & deployment – it’s all about the business
When developing pilots, it’s important to recognize that the organization is addressing a business problem and not just applying a technology. Accordingly, organizations should consider how they can make a process better and achieve service delivery innovation, and not just service delivery automation, before they proceed. One framework that can be used in analyzing business processes is the ‘eliminate/simplify/standardize/automate’ approach.
While organizations will probably want to start with some simple and relatively modest RPA pilots to gain quick wins and acceptance of RPA within the organization (and we would recommend that they do so), it is important as the use of RPA matures to consider redesigning and standardizing processes to achieve maximum benefit. So begin with simple manual processes for quick wins, followed by more extensive mapping and reengineering of processes. Indeed, one approach often taken by organizations is to insert robotics and then use the metrics available from robotics to better understand how to reengineer processes downstream.
For early pilots, pick processes where the business unit is willing to take a ‘test & learn’ approach, and live with any need to refine the initial application of RPA. Some level of experimentation and calculated risk taking is OK – it helps the developers to improve their understanding of what can and cannot be achieved from the application of RPA. Also, quality increases over time, so in the medium term, organizations should increasingly consider batch automation rather than in-line automation, and think about tool suites and not just RPA.
Communication remains important throughout, and the organization should be extremely transparent about any pilots taking place. RPA does require a strong emphasis on, and appetite for, management of change. In terms of effectiveness of communication and clarifying the nature of RPA pilots and deployments, proof-of-concept videos generally work a lot better than the written or spoken word.
Bot testing is also important, and organizations have found that bot testing is different from waterfall UAT. Ideally, bots should be tested using a copy of the production environment.
Access to applications is potentially a major hurdle, with organizations needing to establish virtual employees as a new category of employee and give the appropriate virtual user ID access to all applications that require a user ID. The IT function must be extensively involved at this stage to agree access to applications and data. In particular, they may be concerned about the manner of storage of passwords. What’s more, IT personnel are likely to know about the vagaries of the IT landscape that are unknown to operations personnel!
Reporting, contingency & change management key to RPA production
At the production stage, it is important to implement a RPA reporting tool to:
- Monitor how the bots are performing
- Provide an executive dashboard with one version of the truth
- Ensure high license utilization.
There is also a need for contingency planning to cover situations where something goes wrong and work is not allocated to bots. Contingency plans may include co-locating a bot support person or team with operations personnel.
The organization also needs to decide which part of the organization will be responsible for bot scheduling. This can either be overseen by the IT department or, more likely, the operations team can take responsibility for scheduling both personnel and bots. Overall bot monitoring, on the other hand, will probably be carried out centrally.
It remains common practice, though not universal, for RPA software vendors to charge on the basis of the number of bot licenses. Accordingly, since an individual bot license can be used in support of any of the processes automated by the organization, organizations may wish to centralize an element of their bot scheduling to optimize bot license utilization.
At the production stage, liaison with application owners is very important to proactively identify changes in functionality that may impact bot operation, so that these can be addressed in advance. Maintenance is often centralized as part of the automation CoE.
Find out more at the SSON RPA in Shared Services Summit, 1st to 2nd December
NelsonHall will be chairing the third SSON RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December, and will share further insights into RPA, including hand-outs of our RPA Operating Model Guidelines. You can register for the summit here.
Also, if you would like to find out more about NelsonHall’s expensive program of RPA & AI research, and get involved, please contact Guy Saunders.
Plus, buy-side organizations can get involved with NelsonHall’s Buyer Intelligence Group (BIG), a buy-side only community which runs regular webinars on RPA, with your buy-side peers sharing their RPA experiences. To find out more, contact Matthaus Davies.
This is the final blog in a three-part series. See also:
Part 1: How to Lay the Foundations for a Successful RPA Project
]]>We now turn our attention to Dell Services, which has adopted an automation focus across its life and healthcare insurance BPS processes.
Focusing on healthcare payer & provider and life insurance process automation
In 2016, life insurance accounts for around 30% of Dell Services’ overall BPS revenues and healthcare payer accounts for approximately 35%, with healthcare provider making up the balance. Dell Services takes a platform-led approach to its BPS:
-
It has its own LifeSys platform for life insurance, on to which it migrates a client’s book of business and provides administration services in its own environment; or
-
It partners with a third party supplier for platform capability and tailors it to fit the needs of the book of business, from which it can then provide services, e.g. Dell Services uses partner ikaSystems for its healthcare payer platform needs, on top of which it layers its Dell Business Process Management Suite (DBPMS) tools. The tools include:
-
An enterprise dashboard: including KPI tracking and trend analysis for SLA metrics
-
Client extranet: including an issues log
-
Queue management: including skill-set based routing and priority allocation.
Automation Ideation led by BPS delivery teams
Unlike other providers, who tend to be led by their clients with respect to automation, the process at Dell Services starts with an internal ‘ideas generation’ stage, achieved either through Dell’s ‘LEAP’ (Listen, Engage, Act, Progress) portal where agents are able to log ideas, together with perceived benefits (and are rewarded if their ideas are selected) or via the Business Process Improvement (BPI) team who carry out a ‘click study’ to identify ways in which the process could be re-engineered or automated. In line with its peers, an internal concern about increasing automation was the inevitable change in job composition; for this reason, the LEAP portal is considered particularly important to ensure employees are involved and engaged in driving the initiative forward. In addition, supervisors are targeted with an annual 5%-15% AFTE target. Once an idea has been selected, a feasibility study takes place before the idea is tested and bots are deployed by the central AFTE automation team. Bot management is then passed to the operations team while the bots are monitored through the central bot command center.
Balancing AFTEs with FTEs
In line with the market, Dell Services has concentrated its efforts on applying automation to high volume processes, which account for ~30% to 35% of its overall book of business. To achieve this, it is targeting the introduction of ~300-400 AFTEs year on year, though this is not a static number since clients are on-boarded throughout the year. The overall aim is to achieve around 6% productivity improvement per annum.
Although Dell Services does use third-party RPA platforms, it has developed its own “AFTE” platform incorporated within the Dell Business Process Management Platform. AFTE bots rather than third-party bots are typically deployed where the Dell BPMS platform is already being used or is to be used.
High volume processes (in which AFTEs are being used to varying extents) within each of Dell Services’ insurance services include:
- Life insurance:
- Data entry and indexing: freeing up FTEs to carry out other activities such as policy holder services where less work is typically carried out by AFTEs – though this is something that Dell is looking to change and where Dell is investing in automation initiatives
- Policy issuing: currently, the work is handled 50% by FTEs and 50% by AFTEs, with Dell seeking greater tool maturity before it is able to drive greater automation here
- Premium accounting
- Healthcare payer:
- In-bound calls: FTE-led
- Adjustments: FTE-led
- Adjudication: 50% AFTE, 50% FTE
- Claim processing: FTE-led
- Member enrolment: FTE-led
- Provider maintenance: 50% AFTE, 50% FTE
- Healthcare provider:
- File download: exclusively AFTE
- Medical coding: 50% AFTE, 50% FTE
- Change entry: FTE-led
- Payment posting: AFTE-led
- Credit balancing: 50% AFTE, 50% FTE
- Accounts receivables: FTE-led
A simple example to illustrate some of the quantifiable benefits that have been achieved through automation can be seen through the work that took place to automate call center operations at one of Dell’s life insurance clients. Prior to the introduction of automation, call center agents were required to use a number of screens to capture customer information, which often resulted in comparatively low accuracy, and a high handling time. The system was not user-friendly and baseline training typically took around 10 weeks. Ultimately SLAs were being missed. To address this, Dell condensed the numerous screens into one screen and introduced rule-based processes to ensure no manual calculations were required to complete the form, unlike previously, where up to six manual calculations were required. As a result, AHT fell from 471 seconds to 374 and training took ~7 weeks, as opposed to 10. The quality of data capture increased from 88% to 95% and the average time taken to update notes fell from 110 seconds to 15 seconds¸ because the system was largely able to perform updates itself.
Plans to Implement Machine Learning within Dell BPM Platform
Over the last four years, Dell has extended its capabilities from simple script based-processing, to the development of AFTEs, including an associated AFTE command center. Going forward, the intention is to incorporate a self-learning capability, implement technologies such as NLP and machine learning within the Dell BPMS platform, and to secure end-to-end automation in the processes that are already largely being carried out by AFTEs, e.g. indexing.
]]>
As well as conducting extensive research into RPA and AI, NelsonHall is also chairing international conferences on the subject. In July, we chaired SSON’s second RPA in Shared Services Summit in Chicago, and we will also be chairing SSON’s third RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December. In the build-up to the December event we thought we would share some of our insights into rolling out RPA. These topics were the subject of much discussion in Chicago earlier this year and are likely to be the subject of further in-depth discussion in Atlanta (Braselton).
This is the second in a series of blogs presenting key guidelines for organizations embarking on an RPA project, covering project preparation, implementation, support, and management. Here I take a look at how to assess and prioritize RPA opportunities prior to project deployment.
Prioritize opportunities for quick wins
An enterprise level governance committee should be involved in the assessment and prioritization of RPA opportunities, and this committee needs to establish a formal framework for project/opportunity selection. For example, a simple but effective framework is to evaluate opportunities based on their:
- Potential business impact, including RoI and FTE savings
- Level of difficulty (preferably low)
- Sponsorship level (preferably high).
The business units should be involved in the generation of ideas for the application of RPA, and these ideas can be compiled in a collaboration system such as SharePoint prior to their review by global process owners and subsequent evaluation by the assessment committee. The aim is to select projects that have a high business impact and high sponsorship level but are relatively easy to implement. As is usual when undertaking new initiatives or using new technologies, aim to get some quick wins and start at the easy end of the project spectrum.
However, organizations also recognize that even those ideas and suggestions that have been rejected for RPA are useful in identifying process pain points, and one suggestion is to pass these ideas to the wider business improvement or reengineering group to investigate alternative approaches to process improvement.
Target stable processes
Other considerations that need to be taken into account include the level of stability of processes and their underlying applications. Clearly, basic RPA does not readily adapt to significant process change, and so, to avoid excessive levels of maintenance, organizations should only choose relatively stable processes based on a stable application infrastructure. Processes that are subject to high levels of change are not appropriate candidates for the application of RPA.
Equally, it is important that the RPA implementers have permission to access the required applications from the application owners, who can initially have major concerns about security, and that the RPA implementers understand any peculiarities of the applications and know about any upgrades or modifications planned.
The importance of IT involvement
It is important that the IT organization is involved, as their knowledge of the application operating infrastructure and any forthcoming changes to applications and infrastructure need to be taken into account at this stage. In particular, it is important to involve identity and access management teams in assessments.
Also, the IT department may well take the lead in establishing RPA security and infrastructure operations. Other key decisions that require strong involvement of the IT organization include:
- Identity security
- Ownership of bots
- Ticketing & support
- Selection of RPA reporting tool.
Find out more at the SSON RPA in Shared Services Summit, 1st to 2nd December
NelsonHall will be chairing the third SSON RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December, and will share further insights into RPA, including hand-outs of our RPA Operating Model Guidelines. You can register for the summit here.
Also, if you would like to find out more about NelsonHall’s expensive program of RPA & AI research, and get involved, please contact Guy Saunders.
Plus, buy-side organizations can get involved with NelsonHall’s Buyer Intelligence Group (BIG), a buy-side only community which runs regular webinars on sourcing topics, including the impact of RPA. The next RPA webinar will be held later this month: to find out more, contact Guy Saunders.
In the third blog in the series, I will look at deploying an RPA project, from developing pilots, through design & build, to production, maintenance, and support.
]]>
As well as conducting extensive research into RPA and AI, NelsonHall is also chairing international conferences on the subject. In July, we chaired SSON’s second RPA in Shared Services Summit in Chicago, and we will also be chairing SSON’s third RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December. In the build-up to the December event we thought we would share some of our insights into rolling out RPA. These topics were the subject of much discussion in Chicago earlier this year and are likely to be the subject of further in-depth discussion in Atlanta (Braselton).
This is the first in a series of blogs presenting key guidelines for organizations embarking on RPA, covering establishing the RPA framework, RPA implementation, support, and management. First up, I take a look at how to prepare for an RPA initiative, including establishing the plans and frameworks needed to lay the foundations for a successful project.
Getting started – communication is key
Essential action items for organizations prior to embarking on their first RPA project are:
- Preparing a communication plan
- Establishing a governance framework
- Establishing a RPA center-of-excellence
- Establishing a framework for allocation of IDs to bots.
Communication is key to ensuring that use of RPA is accepted by both executives and staff alike, with stakeholder management critical. At the enterprise level, the RPA/automation steering committee may involve:
- COOs of the businesses
- Enterprise CIO.
Start with awareness training to get support from departments and C-level executives. Senior leader support is key to adoption. Videos demonstrating RPA are potentially much more effective than written papers at this stage. Important considerations to address with executives include:
- How much control am I going to lose?
- How will use of RPA impact my staff?
- How/how much will my department be charged?
When communicating to staff, remember to:
- Differentiate between value-added and non value-added activity
- Communicate the intention to use RPA as a development opportunity for personnel. Stress that RPA will be used to facilitate growth, to do more with the same number of people, and give people developmental opportunities
- Use the same group of people to prepare all communications, to ensure consistency of messaging.
Establish a central governance process
It is important to establish a strong central governance process to ensure standardization across the enterprise, and to ensure that the enterprise is prioritizing the right opportunities. It is also important that IT is informed of, and represented within, the governance process.
An example of a robotics and automation governance framework established by one organization was to form:
- An enterprise robotics council, responsible for the scope and direction of the program, together with setting targets for efficiency and outcomes
- A business unit governance council, responsible for prioritizing RPA projects across departments and business units
- A RPA technical council, responsible for RPA design standards, best practice guidelines, and principles.
Avoid RPA silos – create a centre of excellence
RPA is a key strategic enabler, so use of RPA needs to be embedded in the organization rather than siloed. Accordingly, the organization should consider establishing a RPA center of excellence, encompassing:
- A centralized RPA & tool technology evaluation group. It is important not to assume that a single RPA tool will be suitable for all purposes and also to recognize that ultimately a wider toolset will be required, encompassing not only RPA technology but also technologies in areas such as OCR, NLP, machine learning, etc.
- A best practice for establishing standards such as naming standards to be applied in RPA across processes and business units
- An automation lead for each tower, to manage the RPA project pipeline and priorities for that tower
- IT liaison personnel.
Establish a bot ID framework
While establishing a framework for allocation of IDs to bots may seem trivial, it has proven not to be so for many organizations where, for example, including ‘virtual workers’ in the HR system has proved insurmountable. In some instances, organizations have resorted to basing bot IDs on the IDs of the bot developer as a short-term fix, but this approach is far from ideal in the long-term.
Organizations should also make centralized decisions about bot license procurement, and here the IT department which has experience in software selection and purchasing should be involved. In particular, the IT department may be able to play a substantial role in RPA software procurement/negotiation.
Find out more at the SSON RPA in Shared Services Summit, 1st to 2nd December
NelsonHall will be chairing the third SSON RPA in Shared Services Summit in Braselton, Georgia on 1st to 2nd December, and will share further insights into RPA, including hand-outs of our RPA Operating Model Guidelines. You can register for the summit here.
Also, if you would like to find out more about NelsonHall’s extensive program of RPA & AI research, and get involved, please contact Guy Saunders.
Plus, buy-side organizations can get involved with NelsonHall’s Buyer Intelligence Group (BIG), a buy-side only community which runs regular webinars on sourcing topics, including the impact of RPA. The next RPA webinar will be held in November: to find out more, contact Matthaus Davies.
In the second blog in this series, I will look at RPA need assessment and opportunity identification prior to project deployment.
]]>

At SE2’s Partnership Forum in Boston last week, the main theme was ‘FutureProof’, and specifically how to prepare and guard your company from regulatory and operational uncertainties. In effect, the life and annuities insurance BPS vendor is future proofing itself by investing heavily in its infrastructure, middleware, and platform capabilities to address its own future needs, as explained by CEO Gautam Thakkar and CIO Vinod Kachroo.
Industry drivers
SE2 identified some of the key trends in the insurance industry that will drive the development of applicable offerings, including:
- The need for insurers to provide a continuous income source through annuities, given an aging population; this is particularly challenging in the current low interest rate environment
- The need to approach customers via social media, using effective data manipulation, to enable better decision-making
- Department of Labor (DOL) regulatory changes that will impact clients.
Strategy for growth
In order to achieve future growth, SE2 will focus on greater innovation in its offerings, and enhancing the customer experience to drive better results. Specifically, SE2 is planning to:
- Further invest in data analytics to help identify growth opportunities and operational improvements
- Build RPA and AI capabilities for greater process automation
- Adopt algorithmic underwriting, whereby data aggregation and manipulation will enable automated contract creation for simple policies
- Develop technology and service offerings that address DOL regulatory changes
- Exploit IoT to the extent possible
- Target the millennial and middle-age markets, which have greatest growth potential (as identified in NelsonHall’s Targeting Life, Annuities & Pensions BPS market analysts study earlier this year)
- Increase its use of digitization
- Adopt a ‘direct to consumer’ market approach through omni-channels that simplify the process of insurance buying and administration.
SE2’s roadmap for the coming years also includes a new distributor dashboard, further web enhancements through personalized UIs, efficiency improvements in its call centres, fund automation, and increased use of business rules engines.
To assist it in achieving its goals, SE2 has partnered with:
- NTT Data for infrastructure management and application testing
- Automation Anywhere for RPA
- InRule Technology for business rules management capability
- Informatica for data management and technology transformation.
SE2 is focusing on expanding in the U.S. life market by aggressively increasing its headcount in its New Jersey and Topeka facilities in the U.S., as well as in Waterford in Ireland. It is also looking at potential acquisitions to strengthen its life offerings.
Helping clients meet operational goals
At the forum, SE2 clients Security Benefit Corporation and Global Atlantic described how SE2 is positively impacting their companies’ operational goals. Security Benefit’s CEO, Mike Kiley, stated that his company has continuously increased its policies count and assets under management with the administrative help of SE2, while Global Atlantic’s President and CEO, Nick von Moltke, emphasized the benefit of having a partner that is continually investing in its infrastructure, a key contributor to future success and the ability to adapt to changing market conditions.
A big advantage for SE2 is its sole focus on the insurance vertical. Also, as a private company, it is under less pressure to deliver strong results every quarter. The fact that it operates using its own proprietary platform also distinguishes it from insurance BPS vendors that rely upon third party software to deliver their offerings. These advantages, along with its high employee retention rate, are good indicators that SE2 is well positioned for future growth.
]]>
WNS’ RPA journey is moving quickly, with six pilots underway and five more ready to go. WNS has decided to wait on AI for the time being, in favour of developing its process automation capabilities, which has included the launch of eAdjudicator (a bolt-on RPA tool for claims adjudication) and InsurACE (a policy administration workflow tool) earlier this year.
RPA delivering 25% savings; 40% achievable with employee retraining
Echoing its peers, WNS started by applying RPA to defined, rules-based, and transaction-based insurance activities, specifically in payments and first notice of loss (FNOL), followed by subrogation, since these sub-processes are relatively standardized and do not require human judgement. Based on its pilot experience to date, cost savings in these areas have been around 25%, but in order to realise further cost savings, there is a ‘Phase 2’ that requires re-training of the labor force and process reengineering to take advantage of the automation, which could see a further 10-15% savings. Three of the pilots are in this second phase.
To take its journey forward, WNS required a technology partner who had an insurance focus, a cloud-based offering, and a particular strength in robotics for analytics – specifically with a capability to handle the vast number of compliance requirements imposed by the different U.S. states. It found these in Blue Prism (although it continues to be open to additional partnerships with other technology vendors), who also happened to be looking for more traction in the insurance space – something that WNS brought to the table.
P&C FNOL, Claims & Underwriting the Focus for 2016
In 2016, WNS has three focus areas in which it will be applying RPA, based on client appetite: FNOL, claims processing, and underwriting (UW), with an overall aim of removing the unnecessary steps in each sub-process.
As yet, there does not seem to be huge traction on the life insurance side and, as such, WNS will be focusing on property & casualty (P&C) processes. An example of a recently on-boarded UW client is a U.S. P&C insurer who was seeking to reduce the number of UW assistants it would need to hire. The client expected to hire ~75 UW assistants, but since partnering with WNS, the expectation is now that it will be in a position to hire ~30% less than this, and a further ~20% additional capacity will be created. The client moved from pilot mode for this first line of business (personal auto) to full production in April 2016, and is set to add further lines of business to the scope, each one going through separate pilots.
An example of cost saving achieved through applying the Blue Prism framework to a set of UW processes was with a client whose workforce operated in a predominantly virtual environment. The ‘before’ state saw work passing through ~40 handoffs, which WNS was able to bring down to 7, using workflow mapping. This alone has yielded ~35% savings for the client and has proved ‘transformational’ for the business.
In most cases, the conversations appear to be led by WNS. One of the key concerns raised by clients, however, is around what happens to staff allocation once RPA is deployed. Typically, staff are still very much required, but need re-training to make the most of the new systems and to ensure they operate effectively.
For now, WNS believes that sufficient savings and efficiencies can be gained through applying RPA to an insurance sub-process such as claims logging, which will provide the claims adjuster with a better summation of the situation and enable the handler to carry out the insurance process more effectively and accurately. For example, reducing the number of claims pages down from 50 to 10, and eventually to as little as 7 bullet points of actionable items.
Other similar areas in which WNS has successfully applied this type of RPA include medical review and transcription. However, WNS is of the view that there are some sub-processes that cannot be carried out by anything other than human effort, e.g. bodily injury; as it stands, WNS has not found a way to simulate the experience of the claims handler with RPA for this type of process.
Areas that are now progressed beyond pilot mode and are proving successful for WNS are:
- Vendor payment
- Subrogation (clients are almost all on transaction-based pricing)
- Claims logging
- FNOL (~60% of clients are on transaction-based pricing).
Wipro started its automation journey in the late noughties and has since gone on to set up a dedicated RPA practice, and also developed its own AI platform, Wipro Holmes. Currently, Wipro is principally partnering with Automation Anywhere for RPA software.
Clients showing early interest had questions around which insurance processes bots could most easily be deployed in, and where should they be applying RPA. The processes Wipro found to be most suitable for application of RPA in the insurance sector are claims processing and new business, and hence these are the key focus areas for Wipro.
Efficiency improvements of ~40% in target insurance sub-processes
Today, over 50% of Wipro’s RPA clients are in the BFSI sector, with ~40% using bots for data entry processes and 60% for rules-based services. Wipro currently has four clients for RPA services in the insurance sector split across life, annuities & pensions (LA&P), property & casualty (P&C), and healthcare insurance. Two of these companies are focused on a single geography and two are multi-geography, including U.S., Europe, LATAM and the Middle East.
One of the insurance clients is a Swiss provider of life and P&C services for whom Wipro provides RPA in support of new business data entry. Pre-bots, the filling in of a new business form required the use of multiple unsynchronized screens to collect the necessary information. To address this issue, Wipro developed an interface (a replica of the application form) to enable 100% automated data entry using bots, a typical ‘swivel chair’ use of RPA. This yielded a 30% - 40% efficiency improvement.
In the healthcare payer sector, Wipro has implemented RPA in support of provider contract data management, specifically in the area of contract validation. Here, Wipro designed four bots in 90 days, automating ~75% of the contract validation process and improving productivity by ~40%.
In 2016, Wipro has noticed a shift in customer attitude, with organizations now appreciating the enhanced accuracy and level of auditability that RPA brings.
Of course, the implementation of RPA is not without its objections. One frequent question from organizations just starting the RPA journey is ‘how do I stop bots going berserk if the process changes?’, since once programmed, the bots are unable to do anything other than what they have been programmed to do. Accordingly, Wipro ensures that any changes that occur in a given process are flagged up in the command centre before an attempt is made for them to be carried out by a bot, and a signal is given that the bot needs ‘re-training’ in order to carry out that process.
Secondly, IT departments sometimes ask how long the bots are required to stay in the work environment and how do they fit into an overall IT transformation strategy. Wipro’s response is to treat the bot like an FTE and to keep it for as long as it is achieving benefit, ‘re-training’ it as required. Wipro suggests that bots wouldn’t conflict with the aims of an IT transformation, and ought to be considered as complementary to an IT transformation.
Complementing RPA with Cognitive using Holmes
So far, so good for Wipro regarding its application of RPA in the insurance sector. RPA is being used to address data entry processes (40% of activity) and rules-based transaction processing areas such as claims (60% of current activity). However, this still leaves the question of complementing the rigid process execution of RPA with machine learning and self-learning processes, and also the question of addressing knowledge-based processing requiring human judgment.
This is where Wipro Holmes comes into the picture – a proprietary AI platform with applications for cognitive process automation, knowledge visualization, and predictive services. The platform is not currently being used with insurance clients, but conversations are expected to start within the next 9 months. It is expected that, in contrast to the RPA conversations which were led by Wipro in more than 95% of cases, the AI discussion will be led by existing RPA clients and across a wider pool of services, including finance & accounting (F&A).
Accordingly, the focus now is on developing Wipro Holmes, to ensure it is ready for use with clients in 2017. Insurance activities that will benefit first from this platform could include the area of Know Your Customer (KYC) compliance, to enable more rapid client on-boarding.
]]>If we look at Q4 2015 revenue performance in Cognizant’s two largest vertical groups:
- Financial Services, was up 16.6% to $1,308m, with the strongest growth in insurance
- Healthcare (includes payer, pharma, biotech and medical devices) was up 23.2% y/y to $952m, with the strongest growth in life sciences
These two vertical groups accounted for 70% of Cognizant’s total revenues in Q4, and for 74.5% ($366m) of the company’s overall y/y topline growth.
So why did Cognizant’s share price take a bit of a dive following these results, and furthermore drag down some other stocks with it, before showing some recovery on Friday?
The fact that sequential growth, at 1.4%, was below that reported by Accenture and Infosys may have had something to do with it. At NelsonHall we largely ignore sequential growth, as it ignores seasonality impacts, which may vary slightly from vendor to vendor, depending on their client base.
But the main concern was over Cognizant’s soft guidance for Q1 and full year 2016. Revenue guidance for:
- Q1 2016 is in the range of $3.18bn - $3.24bn, y/y growth in the range of 9.2% to 11.3%
- Full year 2016 is in the range of $13.65bn - $14.20bn, or growth in the range of 9.9% to 14.3%: the expectation is for back-ended growth.
In providing some color on guidance, management highlighted softness in both major vertical groups:
- Financial services, in banking more than insurance, where some of its banking clients are “taking a cautious approach”, putting some projects on hold
- Healthcare, where the major consolidation that is playing out in the payer industry means that some of its larger payer clients are delaying IT plans until their merger plans are clear.
In financial services Cognizant expects to see some level of growth, but given some current project delays in banking, says it is adopting a “wait and see” approach, and until then being conservative in its forecast
In contrast, in healthcare CEO Francisco D’Souza claims to be feeling “very, very good” about the pipeline of large deals Cognizant has for 2016, many of these leveraging TriZetto. The expectation is that healthcare will have a slow start in 2016, with strong growth from H2 and into 2017.
Indian financial and business media was more alarmed by Cognizant’s references to softness in the financial services industry. At one point D’Souza commented “our expectation is that we continue to grow faster than (the) industry… certainly others in the industry I think will probably have some of the same outcomes in financial services that we do”.
In a pointed response to this, TCS issued an investor alert on the Tuesday referring to its own performance in financial services in 2015, pointing out that revenues from the Banking and Financial Services industry vertical in CY 2015 grew by 15% in CC terms, compared with 13.5% CC growth for the company overall, and that, on an organic basis, TCS' CC revenue addition of $1.85bn in CY 15 was “the highest in the industry”. In an interview with India’s Economic Times, TCS CEO N Chandrasekaran claimed “we have not seen anything negative with any client” and that “for financial services as a whole, it is going to be an excellent year for us.”
So why does one major vendor call out softness in BFSI and another major vendor make such positive comments? Has one of them got it badly wrong? Well, clearly not: they are obviously talking to their clients! But a vendor can refer only to its own client base, and to the services they themselves are delivering to that client base. As an indicator of the differences this can mean, where TCS has been suffering headwinds in recent quarters in its insurance business because of its Diligenta BPO unit, for Cognizant, insurance has been the growth engine in its BFSI business recently.
Every vendor today is emphasizing its capabilities in various areas of digital - but it is in the discretionary spend of their clients’ budgets that some vendors are now feeling the pinch. Having a strong outsourcing business delivering recurring revenues is clearly advantageous – and we note that Cognizant’s outsourcing services businesses have been lagging its consulting and technology services businesses, delivering just 7.6% y/y growth this quarter.
This leads us to the other area of softness called out by Cognizant: its healthcare business, which includes payer, pharma, biotech and medical devices. Recent growth has been driven primarily by continued strength in life sciences (which we estimate accounts for about a third of its healthcare revenues) but it is the payer sector that Cognizant has placed its bets, looking to leverage TriZetto to build a BpaaS utility. Cognizant continues to highlight that it is in advanced stages of discussions for some very large deals, that current issues are related specifically to M&A activity, and that it expects some of these deals to close from the second half of this year. To an extent, the consolidation happening in the sector makes a platform-based BPO offering more attractive to buyers. But will Cognizant build a true utility with TriZetto? NelsonHall research shows that while healthcare payers may be amenable to a BpaaS model for some industry-specific activities, as in other sectors, appetite for a true utility service (i.e. a multi-tenant platform model) tends to be low.
Finally, the company continues to generate lots of cash, nearly $700m in Q4, and now has over $4.5bn in cash and equivalents. As well as share repurchase, we may well see further acquisition activity this year, which is, of course, one way of returning to “above industry average” topline growth. It is in the public domain that Cognizant has walked away from negotiations for Dell Services (essentially the former Perot Systems, which has a sizeable healthcare business) because of price. A few weeks ago, Cognizant announced its acquisition of KBACE Technologies; will we see another acquisition announcement in the next few months?
NelsonHall will be updating its Key Vendor Assessment of Cognizant in the next few weeks. This is the most comprehensive profile of Cognizant available on the market. For details, contact [email protected]
]]>HPS' 2015 revenues were $223m. It has achieved a CAAGR of 38% in the last three years, driven both from adding new healthcare payers and from the increase in individuals or groups eligible for first-time insurance coverage due to the ACA initiations; the company now supports ~20% of Individual health plans in the U.S.
The acquisition will be a major boost to Wipro’s ambitions in healthcare and specifically healthcare payer BPS, an area where the company had made modest at best progress since its acquisition of Infocrossing, and the Infocrossing Healthcare Services, Inc. unit in 2007. Wipro Infocrossing currently has healthcare payer BPS contracts with two State Medicaid agencies, including Missouri’s Department of Social Services.
The acquisition of HPS will enable Wipro to move beyond support for the Over 65 market in the form of Medicaid and Medicare, and to address the growing market for individual plans in the Under 65 B2C market. It will provide Wipro with a more modern building block around which to position its healthcare payer BPS business. Such is the importance attached to this building block by Wipro that it is conducting a reverse integration of its healthcare & life sciences business into HPS, with the overall unit being led by HPS' President and CEO Jeff W. Bak.
The Individual policy market is currently a small part of the overall health plan policy base, but it is one that has been showing double-digit growth with the ongoing extension of health insurance coverage in the U.S. Looking at the future dynamics of this market, Wipro expects that the Individual plan member base will continue to grow for the next three years as health insurance coverage of the population continues to expand and will then stabilize. By this point, Wipro perceives that there will be a secondary growth driver for exchanges with health insurance exchange markets becoming attractive to employers as a mechanism for providing health plans to certain groups of employees such as part-time staff.
HPS currently serves ~35 healthcare payers, with its top ten clients accounting for ~80% of its revenues. Its client list includes Ameritas, Allstate, Assurant Health, Beazley, Cigna, Foresters, Humana, Kaiser Permanente, Starmark, UnitedHealthOne, unum, and vsp. HPS’ niche is in assisting healthcare payers to enter and control their costs around state-based and Federal exchanges; it is focused on the ‘individual’/B2C health plan market. HPS has a platform to support healthcare payers across the Individual policy lifecycle and views the typical journey with a healthcare payer in four steps:
- Helping them to connect with private & public exchanges (using its ExchangeLink platform)
- Assisting them in policy administration & member services (ServiceLink platform)
- Helping them with member acquisition through its licensed agents (SalesLink)
- Assisting them in member retention & loyalty (LoyaltyLink).
With these services, HPS can connect healthcare payers to 40 public exchanges and 150 private health insurance exchanges; and the HPS Insurance Agency connects to a network of ~100k nsurance agents. HPS aims to help payers move beyond medical insurance and offer servicing around digital products in other areas such as dental insurance and even life insurance.
HPS has ~2k employees, all onshore U.S. It offers both SaaS and BPaaS services. Clearly the BPaaS element is extremely attractive to Wipro and in line with its strategy for developing its BPS service. HPS will also give Wipro access to a wider client base among commercial healthcare payers and an opportunity to cross-sell wider services such as offshore-centric claims processing while adding credibility to the company’s onshore presence in the U.S. The non-FTE pricing models used by HPS (such as per member per month for member servicing and on a share of premium/commission for new business) will also be attractive to Wipro
Overall, this acquisition will give Wipro both a leadership position in BPS in the Individual healthcare payer market and also the potential for a fresh start in healthcare payer BPS overall, including opportunities to leverage its services around digital and analytics and to start to move into complementary areas such as population health management, patient monitoring, and ACO support. Possible synergies with other analytics offerings should not be excluded, such as with Wipro’s Marvel CX, in order to further enhance customer experience.
Wipro is on a bit of an acquisition spree at the moment: this will be its fourth acquisition so far in FY 16, following those of:
- Designit, which has enhanced the capabilities of Wipro Digital (part of the Change strategy)
- cellent AG, bringing in scale and local relationships in the key European market of Germany
- Viteos Group, bring in BPaaS capabilities in the financial services sector.
Including HPS, Wipro will be making an overall investment of ~$750m in these acquisitions, all of which are strategic, rather than bolt-on, acquisitions. Like Viteos, HPS will afford Wipro the opportunity to build a BPaaS business in one of its principal target sectors.
Footnote: NelsonHall prediction was spot on!
In our January blog on the announcement of the appointment of Abid Neemuchwala as the new Wipro CEO (see here), we said an acquisition like this was highly likely. And in our December 2015 Key Vendor Assessment on Wipro (which will be updated later this week) NelsonHall anticipated that the acquisition spree in FY16 was not finished with Viteos.
If you would like to know more about NelsonHall's extensive coverage of Wipro in our Key Vendor Assessment or any of our IT Services or BPS programs, please contact [email protected]
]]>NelsonHall estimates that the healthcare payer BPS market is worth ~$9.4bn in 2015, and is set to grow at a CAAGR of ~7.6% through 2019, reaching ~$12.6bn in 2019. Of that, we estimate that the government payer market will grow from ~5.3bn to ~7bn, while the commercial payer market will grow from ~4.1bn to ~5.6bn with a CAAGR of ~8.3%.
Health plans are increasingly complying with ACA mandates by trying to provide care to a bigger percentage of the U.S. population, which means that cost reduction is key. There are many opportunities for BPS vendors to help clients reduce costs in areas of intensive manual labor via process automation in both the back office and front office. More than 70% of vendors interviewed by NelsonHall are offering such services, with others planning to do so. There is an increasing tendency to use workflow tools and optimize processes through robotic automation, reducing cost and time in claims management, for example.
Beyond cost reduction, the need for clinical analytics to help improve quality of care is also a key market driver. Healthcare regulations and the ageing long-term care and Medicaid population are driving the need to improve medical management analytics and processes through improving STAR and HEDIS ratings, improving clinical outcomes through use of analytics, improving care management with U.S. qualified nurses, and outcome-based services.
A third key driver is the need to engage members in a more consumer-centric manner. Population health management trends, as well as a changing perception of patients as consumers, means that member engagement offerings are essential for healthcare payers. Relevant services include enrollment, using omni-channel approaches, wellness support, and member engagement through U.S. registered nurses.
According to a panel presentation on healthcare reforms from the global think-tank The Hamilton Group in October 2015, healthcare regulation policies have led to significant decreases in the plan premiums that U.S. insurance consumers pay on average. However, evidence presented showed that patients do not make the optimum choice of health plans when buying insurance. The relative complexity involved in buying insurance in health insurance exchanges (HIX) across the U.S. presents another opportunity for BPS vendors to improve member engagement. Around 40% of vendors interviewed are currently providing such advisory services. These include Concentrix, EXL, HGS and Hewlett Packard Enterprise Services.
Telemedicine, and monitoring long-term care patients from a distance are two more trends on the rise. Xerox has already taken steps in this direction by partnering with HealthSpot, a company providing kiosk-based telehealth services, an alternative to retail and on-site clinics.
In summary, the keys to success in healthcare payer BPS lie in a combination of increased process automation, improved analytics capability, and a more consumer-centric approach.
You can find out much more about what’s driving the U.S. healthcare payer BPS market and about vendors service offerings, as well as understanding the challenges and critical success factors in this market, in NelsonHall’s newly published Targeting Healthcare Payer BPS in the U.S. report.
]]>Capita states it believes the acquisition would:
- Position Capita as a leading provider of technology-enabled BPS
- Provide a stronger platform for Xchanging to accelerate sales growth and to develop its offerings
- Enable Capita to secure £35m+ in cost synergy benefits
- Be immediately earnings accretive.
Capita has been in discussions with Xchanging since early August regarding a possible offer, upping its initial 140p offer to its final 160p proposal on September 24 - which Xchanging’s board confirmed it would be willing to recommend on September 29 should Capita make a firm offer. Capita was granted due diligence access and had until 5pm on November 2 to make an announcenent.
There is another suitor, Apollo, with whom Xchanging has been having discussions about a potential 170p offer. Will this announcement push Apollo into making a counter offer? Xchanging's share price has surged since the news of the potential talks (over 165p at the time of writing, though still below its one-year peak).
Xchanging has been contending with a range of issues, and its global portfolio lacks coherence, partly a reflection of its heritage in a few large and diverse “Enterprise partnerships”. Xchanging is currently between CEOs, Ken Lever having announced his intention in July to step down at the end of the year, and new CEO Craig Wilson not yet started.
If Capita were to complete, this would be its largest ever acquisition, dwarfing its second largest, the £157m acquisition of avocis this February (though there have been a number of £50m+ acquisitions since 2011, helping Capita expand into new markets or extend its IT capabilities). So why is Capita so interested?
In recent years, Xchanging has repositioned and invested to emphasize its capabilities in “technology-enabled BPS”- exactly what Capita is emphasizing with its own various BPO offerings. Also, the private sector is increasingly important to Capita (over 60% of its current pipeline is in commercial sectors) and Xchanging would increase its presence in the Lloyds market, where Capita already has a presence for specialist services.
Looking in more detail at Xchanging assets that would be attractive – or at least very relevant - to Capita:
- Xuber software suite for the non-life commercial market: the biggest investment to date (a whopping $200m+ in total investments since 2011), both in platform development and in acquisitions: in 2014, Xchanging invested £75.6m in acquiring Total Objects, whose binder software is now integrated into the Xuber suite, and Agencyport Europe,extending its software into the health insurance sector, with software for international private medical insurance and exposure modeling (acquisition was delayed), plus a further £11.7m on development of Xuber. Xchanging has found converting interest in Xuber to sales more challenging than anticipated, particularly in the U.S. Will Capita’s greater commercial clout help? It would inherit sales teams from Xuber, Total Objects and Agencyport Europe that need integrating into a single unit to cross-sell, where relevant, the portfolio. Would Capita place the Xuber business in its newest operating division “Capita Digital and Software Solutions”, or would it place it in an insurance sector division?
- The Xchanging Claims Services BPS unit : Capita is already active with a range of specialist services in the London insurance market: this capability would neatly expand its portfolio
- Xchanging’s business in Germany, where it provides investment account administration BPS for Fondespot Bank, will also be of interest to Capita, who is building a presence in the DACH region, via an acquisition spree in the CMS BPS market, also via an insurance BPS contract with Zurich. The complex administration services in Germany that Xchanging would bring in to Capita would fit well in its Asset Services division
- Procurement: Xchanging has been through a significant change of direction with its procurement services in recent years, to technology-led offerings, boosted by the acquisitions of MM4 (which was U.S centric) and Spikes Cavell Analytics Ltd (SCAL, which was U.K public sector centric). These offerings may find traction in the Capita client base
- Expanded offshore IT services capabilities: in India, Xchanging has centers in Chennai and Pune, Bangalore, and tier 3 cities such as Shimoga (Karnataka). It also has a center in Kuala Lumpur, Malaysia, most providing IT infrastructure services to YTL Communications, and a smaller ADM unit in Singapore (where Capita also has a small presence, targeting the reinsurance sector). There is also some offshore BPO activity in India and Malaysia. Capita may rationalize some of these sites, but would certainly be interested in the expanded offshore application services and BPO delivery capabilities
- IT services: Xchanging has some networking capabilities, with a client base in the education and health sectors, as well as Lloyds – this would fit well into the Capita IT Enterprise Services division, which has grown through a series of acquisitions in recent years
And less attractive to Capita?
- The Australian operations, where Xchanging’s New South Wales Workers’ Compensation contract was not renewed, and where its procurement business has not really gained traction.
- The U.S. business: Capita’s international efforts are currently focused on Northern Europe. It would be a major change of strategy for Capita to start targeting the U.S., and its management will be highly aware of other service providers who have tried and failed to penetrate the U.S.
But overall, Xchanging’s portfolio is particularly well suited to Capita's business and where it is looking to develop over the next few years. And the cost synergies from the head office rationalization are also a particularly good match.
We thus believe is highly unlikely that, even if there is a higher counter offer from Apollo, the Xchanging board will change it recommendation to shareholders: Capita presents a better option longer term. Howver, a counter offer from another IT services vendor might be more attractive.
NelsonHall has just published a comprehensive Key Vendor Assessment on Capita. We have also historically included Xchanging in the KVA program.
]]>- Revenue was $4,817m, down 15.5% y/y, and down 10% in constant currency (CC), reflecting key account run off and weakness in EMEA
- Segment earnings before taxes (EBT) were $194m, a margin of 4.0%, up 143 bps y/y.
Q2 FY 2015 revenue by service line (with y/y revenue growth) was:
- IT Outsourcing $2,871m (-20.2%, -10% in CC)
- Applications and business services $1,946m (-7.6%, -2% in CC).
HP ES contributed 18% of HP Group revenue and 8% of Group EBT (up from 5% last quarter)
HP Group is nearing the completion of its 2012 restructuring plan. In Q2 FY 15, ~3.9k people exited HP making the total reduction to-date ~48k. The program has a total of 55k people expected to exit by the end of FY 2015, so a further 7k departures over the next two quarters.
HP has maintained full FY 2015 guidance for Enterprise Services of a revenue decline of between 4% and 6% on a constant currency basis, with an improvement in H2.
So where are the positives in HP ES' performance this quarter?
- A significant improvement in revenue performance in the Apps and Business Services segment, with a CC y/y decline of just 2%. This is led by the BPO business. And some geos are showing flat to slight CC growth
- Signings were up year over year, even without the $2bn Deutsche Bank deal closed at the beginning of the quarter (see our commentary here).
- And “Strategic Enterprise Services” signings continue to grow.... though no details are provided.
But the problems continue at HP ES’ ITO business. It not only continues to be impacted from contract runoff from three large accounts continues, but is also being challenged by the evolution in the market. Meg Whitman refers to “risk in the longer term sustainability of this profit level if we don’t do further cost reductions”. As such, the current intention is to streamline HP ES and take up to $2bn of gross annualized costs out of the business over the next three years in pursuit of a longer term EBT margin target of 7% to 9%. The likely charge represents around 9% of HP ES overall revenues - and 14% of the revenues of the ITO business.
The restructuring actions in HP ES and in particular ITO will include initiatives such as further offshoring, data center automation, pyramid management… the same actions highlighted by CSC earlier this week.
Nevetheless, Whitman has made a clear statement of commitment to the future of HP ES: "the Services business in ES - (and the) - TS Consulting businesses are becoming more strategic to the future of Hewlett-Packard Enterprise…. “increasingly, services is becoming the tip of the spear”.
]]>A year later, EXL delivered full year 2014 revenues that beat revised non-GAAP guidance by $11.6m, finishing the year with 9% growth in Q4, bolstered by better than expected contribution from the recently acquired Overland Solutions (OSI, $12.2m, against the anticipated $10m).
By service type,
- The newly named Operations Management segment (formerly ‘Outsourcing’), continues to represent over three quarters of total revenue and was up 2.7% y/y, or 11% excluding disentanglement costs
- The ‘Analytics and Business Transformation’ segment delivered double digit topline growth every quarter, and 31.9% growth in 2014 overall, reaching $110.6m. EXL’s analytics services business grew 44% in 2014, and now account for 13% of revenue, or $66m. Including contributions from its latest acquisition, RPM Direct, EXL expects its analytics business to reach over $100m in annual revenue in 2015 (or ~20% of total revenue).
Though details of the ‘new EXL’ won’t be revealed until the Investor Day next week, the journey that has been made by EXL this year has been marked by three specialist acquisitions within seven months, the third announced only this week.
- The spending spree started off reasonably small, with Blue Slate Solutions last July for $7m. Blue Slate generates ~85% of its revenues from health insurers (including Medicare contractors) and brings with it a consulting framework that EXL is integrating into its BPO and healthcare technology and analytics capabilities. Blue Slate brought to EXL a specialist onshore staff with domain experience in the U.S. health insurance sector
- The October acquisition for $53m of OSI further added to EXL’s onshore delivery network in the U.S. and to its BPaaS offerings for P&C, particularly in workers’ compensation premium audits
- These two acquisitions will bring in over $105m incremental revenue in 2015, more than offsetting the headwind of ~$49m from transitioning clients. As well as onshore resources, both have developed proprietary tools and frameworks to support their service delivery
- The third acquisition, yet to be completed, is of RPM Direct (for $47m in cash plus earn outs of up to $23m). RPM Direct will enhance EXL’s marketing analytics capabilities in U.S. insurance, across P&C, life and health segments. EXL had indicated a year ago that marketing and customer analytics are focus areas within its “Decision Analytics” services unit. RPM will broaden the range of services EXL can offer to insurance sector clients
All in all, EXL will have invested over $130m in these three acquisitions, all of which
- Boost its onshore presence in the U.S
- Bring in IP (tools, frameworks, marketing database)
- Bring in specialist domain capabilities in the health payer and other insurance sectors
- Broaden its U.S. client base.
Looking ahead to 2015, EXL has given revenue guidance of $570m to $590m, excluding any impact of RPM, a growth rate of 8.5% to 12.5%. Q1 is the last quarter where revenue headwinds from transitioning clients will have a significant effect.
EXL is developing analytics CoEs, particularly in support of healthcare and insurance and is expecting to sign a number of $10m plus annual revenue clients. Will we see further tuck-in acquisitions to further expand its capabilities in different areas of analytics for insurance and healthcare in 2015? The indications are that this is very possible.
EXL started emphasizing its analytics offerings around 18 months ago: at the time, much of the portfolio was based on India delivery. EXL today has a much richer portfolio to offer in its target verticals in the U.S.
Meanwhile, the U.K. , which accounts for over 20% of global revenues, delivered a strong year; EXL does not provide constant currency growth figures, but reported revenue growth for the U.K. in 2014 was 10%, all of which organic. Were EXL’s spending spree to continue into 2015, maybe U.K./EMEA will come higher up its investment priorities.
Finally, EXL has authorized a three-year $20m annual share repurchase program to offset share dilution from annual employee equity grants.
We note that EXL’s share price is at its highest for over two years and has surged by ~20% since the beginning of the month.
By Fiona Cox and Rachael Stormonth
NelsonHall will be producing its first ever Key Vendor Assesment on EXL in March.
]]>The acquisition will enhance Accenture’s digital capabilities in analytics, cloud and mobility for federal agencies. It also will add agile delivery expertise. Agilex brings in capabilities in agile software development for digital solutions. The company currently serves a number of federal departments and independent agencies, such as the VA, DoD, DHS, and Department of Commerce. Commercial sector clients have included Amtrak.
Agilex was founded in 2007 by the late Robert La Rose (who had previously founded Advanced Technology Inc. and Integic, both of which were subsequently acquired), Jay Nussbaum (ex. Citibank and Oracle) and John Gall and quickly attracted senior talent to its leadership. The company offers services around
- Mobile applications for activities such as field inspection, emergency response management, performance dashboards, biometric identification, asset management, case management, personal productivity, etc.
- Healthcare IT - for example Agilex was involved in the deployment of the NHIN CONNECT Gateway. Also m-health - for example in May 2014 it was awarded a contract by the VA to develop and implement an enterprise web and mobile application image viewing solution
- CRM solutions.
Agilex has grown from 20 employees in 2007 to about 800 today. Nussbaum and Gall will leave when then acquisition closes, while the company’s leadership team will be integrated into AFS.
So why the acquisition?
- AFS is already one of the largest U.S. federal systems integrators – this is about continuing to evolve its capabilities to be at the forefront of newer areas of demand; quite simply, Agilex brings in capabilities around digital technologies – and digital is clearly among the top priorities of the government sector
- And governments, not just in the U.S., are looking with much more interest in agile delivery as they move away from massive monolothic projects (for example, agile delivery has been a key element in the U.K. in the development of a new Universal Credit system for the DWP)
Accenture’s 2013 acquisition of ASM Research expanded its presence in the military healthcare market (DoD and VA) - and Accenture has worked alongside Agilex in projects at the VA.
]]>However, IBM is in the midst of a major adjustment of its portfolio. In line with this, the company is reporting $25bn in revenues (and 16% revenue growth) in 2014 (out of a total of $92.8bn) from its "strategic imperatives". IBM's acquisition of Softlayer, where it continues to invest strongly, appears to be delivering $3.5bn annual "as-a-service" run rate and IBM reports that its "Cloud" business had 2014 revenues of $7bn and 60% revenue growth (this includes hardware, software and services),
The revenue growth reported from IBM's other "strategic initiatives" were:
- Analytics +7% (2014 revenue approx $17Bn)
- Security +19%
- Mobile >200%.
Maintaining a high mix of software remains important to IBM but its strategy is now much more nuanced than the simplistic "software good" strategy the company sometimes appeared to adopt in earlier years, with the company rediscovering success in IT infrastructure management. Indeed IBM's acquisition of SoftLayer and its ongoing investment in Cloud infrastructure including in additional in-country SoftLayer data centers and cloud enablers such as security and its Bluemix cloud development platform is arguably having more impact on its signings than any of its investments outside Watson and analytics. In Q4, IBM's cloud infrastructure business moved way beyond the standard fare of IaaS contracts with start-ups to facilitating major infrastructure transformation contracts with values of a $1bn+ with the likes of Lufthansa and WPP.
Indeed, while the impact of SoftLayer was insufficient to lead to material growth in IBM's outsourcing revenues in Q4 2014, its impact is certain to be felt on outsourcing revenue growth in 2015 as a result of these and additional major transformations to cloud infrastructure. Led by these deals, IBM's outsourcing signings transformed in Q4 2014, up 31% (in constant currency and adjusted for disposals). IBM now just needs its application management business, which is continuing to decline under competitive pressure, to undergo a similar transformation.
]]>The NelsonHall Vendor Evaluation and Assessment Tool (NEAT) for P&C BPO in the automotive sector is now available to NelsonHall clients, and is also available for a period free-of-charge to buy-side organizations through NelsonHall and through its partners SIG and SSON.
The tool covers a number of P&C BPO business situations, including the provision of end-to-end P&C BPO processes for the automotive sector, specific focus on claims process improvement, reduction of customer churn through improved service levels, and activity in support of improving the underwriter’s use of time and efficiency.
Suppliers of P&C BPO in the automotive sector covered by this NEAT evaluation include CSC, Cognizant, EXL, Genpact, Infosys, Innovation Group, MphasiS, Quindell, Sutherland, TCS, and WNS.
The NEAT tool for P&C BPO in the automotive sector is part of NelsonHall’s “Speed-to-Source” initiative. The tool sits at the front-end of the vendor screening process and consists of a two-axis model: assessing vendors against their “ability to deliver immediate benefit” to buy-side organizations and their “ability to deliver innovation in support of client-specific requirements”.
The NEAT evaluations are based on a combination of interviews with the vendors and their clients. The vendors are scored against a wide range of criteria, establishing a number of scenarios, each representing a different business situation or client business need.
To add further value, the NEAT tool enables buy-side organizations to input their own weightings and tailor the P&C BPO dataset to their specific requirements across 40 individual vendor evaluation criteria. Using the interactive web-based tool, sourcing managers can configure the NEAT evaluations in accordance with their own priorities and business requirements for service offerings, delivery capability, customer presence, benefits achieved, and other criteria.
]]>In its early days, BPO was a linear and lengthy process with knowledge transfer followed by labor arbitrage, followed by process improvement and standardization, followed by application of tools and automation. This process typically took years, often the full lifetime of the initial contract. More recently, BPO has speeded up with standard global process models, supported by elements of automation, being implemented in conjunction with the initial transition and deployment of global delivery. This timescale for “time to value” is now being speeded up further to enable a full range of transformation to be applied in months rather than years. Overall, BPO is moving from a slow-moving mechanism for transformation to High Velocity BPO. Why take years when months will do?
Some of key characteristics of High Velocity BPO are shown in the chart below:
|
Attribute |
Traditional BPO |
High-Velocity BPO |
|
Objective |
Help the purchaser fix their processes |
Help the purchaser contribute to wider business goals |
|
Measure of success |
Process excellence |
Business success, faster |
|
Importance of cost reduction |
High |
Greater, faster |
|
Geographic coverage |
Key countries |
Global, now |
|
Process enablers & technologies |
High dependence on third-parties |
Own software components supercharged with RPA |
|
Process roadmaps |
On paper |
Built into the components |
|
Compliance |
Reactive compliance |
Predictive GRC management |
|
Analytics |
Reactive process improvement |
Predictive & driving the business |
|
Digital |
A front-office “nice-to-have” |
Multi-channel and sensors fundamental |
|
Governance |
Process- dependent |
GBS, end-to-end KPIs |
As a start point, High Velocity BPO no longer focuses on process excellence targeted at a narrow process scope. Its ambitions are much greater, namely to help the client achieve business success faster, and to help the purchaser contribute not just to their own department but to the wider business goals of the organization, driven by monitoring against end-to-end KPIs, increasingly within a GBS operating framework.
However, this doesn’t mean that the need for cost reduction has gone away. It hasn’t. In fact the need for cost reduction is now greater and faster than ever. And in terms of delivery frameworks, the mish-mash of third-party tools and enablers is increasingly likely to be replaced by an integrated combination of proprietary software components, probably built on Open Source software, with built in process roadmaps, real-time reporting and analytics, and supercharged with RPA.
Furthermore, the role of analytics will no longer be reactive process improvement but predictive and driving real business actions, while compliance will also become even more important.
But let’s get back to the disruptive forces impacting BPO. What forms will the resulting disruption take in both the short-term and the long-term?
|
Disruption |
Short-term impact |
Long-term impact |
|
Robotics |
Gives buyers 35% cost reduction fast |
No significant impact on process models or technology |
|
Analytics |
Already drives process enhancement |
Becomes much more instrumental in driving business decisions Potentially makes BPO vendors more strategic |
|
Labor arbitrage on labor arbitrage |
Ongoing reductions in service costs and employee attrition
|
“Domestic BPO markets” within emerging economies become major growth opportunity |
|
Digital |
Improved service at reduced cost |
Big opportunity to combine voice, process, technology, & analytics in a high-value end- to-end service |
|
BPO “platform components” |
Improved process coherence |
BPaaS service delivery without the third-party SaaS |
|
The Internet of Things |
Slow build into areas like maintenance |
Huge potential to expand the BPO market in areas such as healthcare |
|
GBS |
Help organizations deploy GBS |
Improved end-to-end management and increased opportunity Reduced friction of service transfer |
Well robotics is here now and moving at speed and giving a short-term impact of around 35% cost reduction where applied. It is also fundamentally changing the underlying commercial models away from FTE-based pricing. However, robotics does not involve change in process models or underlying systems and technology and so is largely short-term in its impact and is a cost play.
Digital and analytics are much more strategic and longer lasting in their impact enabling vendors to become more strategic partners by delivering higher value services and driving next best actions and operational business decisions with very high levels of revenue impact.
BPO services around the Internet of Things will be a relatively slow burn in comparison but with the potential to multiply the market for industry-specific BPO services many times over and to enable BPO to move into critical services with real life or death implications.
So what is the overall impact of these disruptive forces on BPO? Well while two of the seven listed above have the potential to reduce BPO revenues in the short-term, the other five have the potential to make BPO more strategic in the eyes of buyers and significantly increase the size and scope of the global BPO market.
Part 1 The Robots are Coming - Is this the end of BPO?
Part 2 Analytics is becoming all-pervasive and increasingly predictive
Part 3 Labor arbitrage is dead - long live labor arbitrage
Part 4 Digital renews opportunities in customer management services
Part 6 The Internet of Things: Is this a New Beginning for Industry-Specific BPO?
]]>|
Sector |
Examples |
|
Telemedicine |
Monitoring heart operation patients post-op |
|
Insurance |
Monitoring driver behavior for policy charging |
|
Energy & utilities |
Identifying pipeline leakages |
|
Telecoms |
Home monitoring/management - the "next big thing” for the telecoms sector |
|
Plant & equipment |
Predictive maintenance |
|
Manufacturing |
Everything-as-a-service |
So, for example, sensors are already being used to monitor U.S. heart operation patients post-op from India to detect warning signs in their pulses, while a number of insurance companies are using telematics to monitor driver behaviour in support of policy charging. Elsewhere sensors are increasingly being linked to analytics to provide predictive maintenance in support of machinery from aircraft to mining equipment, and home monitoring seems likely to be the next “big thing” for the telecoms sector. And in the manufacturing sector, there is an increasing trend to sell “everything as a service” as an alternative to selling products in their raw form.
This is a major opportunity that has the potential to massively increase the market for industry-specific or middle-office BPO way beyond its traditional more administrative role.
However, it has a number of implications for BPO vendors in that the buyers for these sensor-dependent services are often not the traditional BPO buyer, these services are often real-time in nature and have a high level of requirement for 24X7 delivery, and strong analytics capability is likely to be a pre-requisite. In addition, these services arising out of the Internet of Things potentially take the meaning of risk/reward to a whole new level, as many of them potentially have real life or death implications. Some work for the lawyers on both sides here.
Coming next: High-Velocity BPO – What the client always wanted!
Previous blogs in this series:
Part 1 The Robots are Coming - Is this the end of BPO?
Part 2 Analytics is becoming all-pervasive and increasingly predictive
Part 3 Labor arbitrage is dead - long live labor arbitrage
Part 4 Digital renews opportunities in customer management services
]]>On the plus side, there has also been a number of significant wins, the most recent of which was announced yesterday, and Quindell is back on the up as we move into the final months of 2014. In fact, it was almost exactly a year ago that Quindell won a major deal which set the tone for things to come. That win was in the Canadian telematics market, and marked a first North American contract for Quindell when, in November 2013, it was awarded a five-year contract by CAA South Central Ontario, for whom it now provides its telematics technology.
Then, in February 2014, Quindell increased its share in U.K. telematics company ingenie from 43% to full ownership, making Quindell a ‘one-stop-shop’ for auto insurance, with service provision now covering:
- Full scope BPO services: aided by its acquisition of Ai solutions
- Health services: also built up through acquisition of ACH Group in January of this year
- Legal services: including personal injury services for road traffic accidents
- Analytics across the board.
The ingenie product is a telematics box, the size of a smart phone, which includes:
- A GPS unit to capture when and where the car is driven
- High frequency motion sensors which capture how the car is driven
- A SIM card which is used to transmit the data via the EE network.
It is not new technology (it has been used for many years in commercial vehicles), but telematics is the ‘analytics of the moment’ in auto insurance and since drivers remain largely price sensitive, (and telematics boxes enable cost of premiums to be more aligned to performance), they will undoubtedly become much more widely used by car drivers.
At the time of its acquisition of ingenie, Quindell said that telematics insurance systems were that the heart of its growth strategy in technology. The first part of the strategy was to launch an ingenie-based driver product in Canada, which in April 2014 almost happened when Quindell and RAC formed a JV to create ‘Connected Car Solutions’ (CCS). Services were to be delivered from July 2014 in the U.K. and Canada, and outside the age bracket of 17-25 year olds. However, in September 2014, it was announced that Quindell would be buying back the RAC’s shares in CCS, with associated restructuring cost of £3.5m to Quindell payable over 18 months. Following a sharp dip in Quindell’s share price, the warrants that the RAC had received in exchange for its part in the deal, were rendered useless – having once been worth ~£125m.
But now comes the good news: a contract win, announced yesterday, with Aviva Canada. Aviva has also had an interesting relationship with telematics. In 2005, Aviva Canada was the first Canadian insurer to introduce a telematics based auto insurance scheme, Autograph, but this was subsequently disbanded in August 2011 largely owing to cost. Likewise in 2008, Aviva U.K., through its Norwich Union subsidiary, also folded its PAYD offering due to a lack of interest. But now, with costs coming down and customers showing increasing appetite for usage based insurance (UBI) services, Aviva is taking a second stab at telematics, but this time, to some extent, plaingy catch up with its peers who have been offering PAYD and UBI services for some time.
Having re-entered the telematics market gently in mid-2012 with a simple mobile app (rather than through installation of black box technology), Aviva Canada, already a client of Quindell, will now be exclusively using Quindell’s telematics technology to support both commercial and personal LOBs (see NelsonHall Tracking Service article for further contract details).
In May this year, Quindell and Independent Broker Resources Inc. (a wholly owned subsidiary of the Independent Brokers Association of Ontario (IABO)) outlined a two pronged telematics growth strategy for the Canadian market:
- Via ingenie: expansion into the Canadian marketplace with a telematics product for 16 to 24 year olds to be distributed exclusively through member brokers of the IBAO
- A IBRI/Quindell general telematics offering that allows insurers to provide a broker-branded telematics service.
Until yesterday, Quindell had launched two pilot programs for the second option, and a further 17 NDAs had been signed with insurers across Canada. With the addition of the Aviva contract, Quindell’s telematics technology can be sold directly though the 1.7k Aviva Canada brokers.
This, coupled with the CAA win last year, puts Quindell in a strong positon to exit 2014; it also demonstrates that any potentially damaging noise from earlier in the year is not impacting Quindell’s ability to win business. At close of play yesterday, Quindell’s share price was up 9.6%.
]]>First CEO TK Kurien opened by describing Wipro’s view of the market:
- Enterprises were created prior to the current digital era. As a result, customers cannot engage easily or effectively with legacy enterprises operating with old style operating models and operations systems
- Operations vendors (IT services and BPO) will be disrupted. “Slow and certain”, Wipro’s previous model, where offerings were developed and tested to assure quality outcomes, is no longer a successful strategy. Wipro describes its current model as “Fast and Uncertain”, where ideas are tried, then adapted over time, as a flexible strategy more appropriate for rapidly changing times
- The journey with clients to a digital operational development cannot be undertaken at full maturity. It requires Wipro, partners, and clients to slowly adapt while also continuing to provide current services. To accomplish that Wipro needs to maintain and aggressively grow existing operational relationships. Wipro will aggressively pursue new business to establish larger market share, because existing clients provide a base from which transformation can be launched (i.e., upsell). Kurien did not discuss how he intends to pursue new business before transformation. Presumably aggressive pricing and terms would underpin such a grab for marketshare
- Traditional BPO will be disrupted, with value levers extending beyond labor arbitrage and simple process re-engineering. While this has been a theme for several years in the industry, Kurien indicated community sourcing (open source software, cloud computing, and shared services) as opposed to vendor specific offerings will drive enterprise operations much more so in the years ahead than has been the case to date.
To address these trends, Wipro is changing its own approach. Key initiatives include:
- Digital POD, Wipro’s methodology for clients designing new operations environments (both platforms and processes).The process draws on strategy, design, and technology. Wipro is building technology and design capabilities in concert with partners to support clients’ evolving business strategies. Specifically Wipro is currently building three digital POD centers in London, Bangalore, and the Bay area of California. These centers will work on client engagements designing new operations environments for clients. As examples of how this might work, Wipro referred to several tier one banking clients, hit hard by the financial crisis and culling businesses and operations, who are redefining their business models to adapt to changing regulations and competitive conditions. Automating manual processes, modernizing legacy platforms, and maintaining ongoing delivery requires third party help from a combined IT/BPO vendor. An early example of what Wipro wants to do, according to Kurien, is a top 4 bank in the U.K. that Wipro has helped over the past three years improve its retail customer support using platform and operations change and support. During that time the client moved up from fourth to first in customer satisfaction ratings.
- Alliances and partnerships:
- Open source: Wipro has committed to invest over the next two years to further develop its open source capabilities. Open source development has become a key area of investment for banks and other global 100 companies. Open source is used by enterprises for its low cost and ability to deliver custom functionality.
- Wipro is building on its existing experience and joining open source communities to better identify best resources, also to help formulate community priorities
- Corporate VC fund to invest in tech start-ups. Wipro has made three investments so far
- Move its own business model from labor arbitrage to process arbitrage (global standardization and greater automation of processing). Wipro has seen their clients’ focus for operational change shift from cost of resource to total cost of ownership (TCO), over the past few years and believes this trend will continue and accelerate.
Wipro articulated that, as a company, it is responding to the fact that businesses in its target sectors (banking, healthcare and retail, to name just three) are having to change their entire operational delivery methodology to adapt to the changing environment. Wipro also highlighted that this requires to talent - both technology and operations talent.
And, like many other IT services providers, Wipro is looking with increased interest at alliances and partnerships. Partnering however requires a wide net to succeed. Most partnerships are weak, some are strong, and a few drive strong value creation.
The challenge with partnering is how to drive partners forward to execution when they have competing demands/opportunities. Successful partnerships require the alignment of goals and culture, which in turn requires due diligence on potential partners and clear signalling of intentions and values.
Participation in communities, such as open source, is table stakes to access and due diligence, but not the trigger to execution. Wipro has indicated it will support partners by identifying sub-domains where it will be active. Wipro has a large client base, something developers typically do not. Wipro can create a market for open source developers’ services, while providing its clients with quality assurance and scale. IT and operational support. In the long run, we believe Wipro will need to selectively partner with relatively few organizations and people for open source capabilities. Ultimately, Wipro will need large scale in-house complementary resources to capitalize on engagements. Leveraging the independent resources of alliance partners to deliver operational change to clients will demand that Wipro bring its own operational scale to the table, not merely IT skills.
]]>NIIT has delivered IT services to its Lloyds of London clients for some 20-years, using its insurance specific tools:
- Subscribe: NIIT’s existing policy administration platform, a multi-currency insurance and reinsurance policy administration system
- Exact Advantage: a data capture facility for property, terrorism, credit risk, aviation and marine. The tool is used to assess and monitor risk exposure, using a mapping interface and GIS technology
- Ipf3: process automation and workflow tool
- Acumen Advantage: provides management information, encompassing underwriting, claims, reinsurance accounting and actuarial data.
Over the years, NIIT has enhanced these tools and also made acquisitions such as Room Solutions in 2006 (see separate article) in support of its insurance business.
In anticipation of new opportunities in the P&C insurance sector, stemming from a combination of factors (see below), NIIT is now launching a suite of software which combines all these tools, also a new tool.
The new product is intended to help commercial insurers deal with the challenge of operating with multiple systems: NIIT’s insurance clients, for example, typically operate with around a dozen systems, each with different regulatory and LOB capabilities. The new platform enables the effective integration of these systems by operating as an overriding core platform, while allowing clients keep the individual reporting processes of the various PAS, and the specific functionalities for different LOBs (some in the London market being particularly specialist).
The new product allows NIIT to address some of the key issues faced by insurers today, including:
- Increasing regulatory requirements
- Ongoing M&A activity: insurers continue to acquire books of business which operate on different PAS. A system that enables the assimilation of additional systems gained through acquisition is likely to be attractive; it also removes the need for training on different PAS and requires knowledge of just one system.
NIIT has between 15 and 20 clients operating on its existing Subscribe system currently and anticipates that all its clients will ultimately move onto the new platform. The first wave of client switch over is under way with two clients in PoC trials and a third in a model office. In effect, the move from Subscribe is an upgrade and the cost of switch over will be picked up by the client.
NIIT will continue to maintain Subscribe for a minimum of five years, as users migrate onto the new platform. NIIT is about to make improvements to Subscribe to ensure it is kept technically up to date - improvements will include replacing the Adelphi front-end and bringing the back-end up to a modern version of Sequel.
A major difference is that Subscribe is a post-bind system, running processes after submission and quotation, whereas, the new platform is a pre-bind and post-bind system starting at the point of initial case creation and running through to pricing.
Bringing its various insurance software tools and applications under one umbrella will help raise the profile of NIIT’s insurance solutions. The official launch of the new platform is October 1, 2014.
]]>TriZetto has a headcount of 3.7k (Cognizant at end of H1 2014: 187k.4). In its last 12 months, TriZetto had $711m in revenues and a non-GAAP operating margin of 18.4% (Cognizant in 2013: 20.6%).
TriZetto LTM revenues breakdown by service/product line is:
- Payer software: 40% (~$277m)
- Consulting: 23% (~$164m)
- Hosting: 13% (~$92m)
- BPO: 5% (~$36m). BPO services are provided on the Payer side
- Provider SaaS: 20% (~$142m).
Cognizant has higlighted the acquistion of TriZetto as an important step in the company's history:
- Towards a non-linear growth business. TriZetto is obiously an ISV business and has higher revenue per head (~$190k) than Cognizant (~$50k). Howevever, Cognizant is not buying a provider of plartforms: TriZetto is essentially a traditional ISV selling on premise perpetual licenses, where applications are implemented and customized by the client
- SaaS revenues represent 20% of revenues, BPO services 5% only - As a revenue generator with planned $1.5bn in additional revenues over 5 years. TriZetto has been a flat growth vendor overall in spite of M&As. In addition, the additional $1.5bn in additional revenues does not mean that Cognizant will triple revenues of TriZetto. Taking an assumption of revenue synergies happening towards the endof this 5-year period, TriZetto could reach sales of ~$1.3bn, up from $700m currenly. This is nice but hardly exponential for the company of the quality of Cognizant
- TriZetto with its software product business has high margins. Yet, TriZetto has lower operating margins than Cognizant. In addition, TriZetto under the ownershipby Apax Partners, offers little cost synergies. This means that under Cognizant, which will be focusing on revenue growth and investment in sales and products, the operating margin of TriZetto is likely to go down.
This lack of growth raises the question of price. Cognizant has not provided detailed information regarding its net profitability. Yet $2.7bn in cash for a company with flat revenues at best, a net profit likely to be in the $70m-$100m range and no cost synergies expected seems a bit expensive. However the market seems comfortable with the price Cognizant paid for TriZetto: Cognizant's share price was relatively flat after the annoucement.
This acquistion will put on hold any other significant M&A for Cognizant for while as the company will be focusing on small tuck-in acquistions to strengthen specific capabilities and focus on share buy-backs.
]]>