
In recent discussions with WNS, NelsonHall explored the company's advanced healthcare management solutions. WNS provides evidence-based criteria to guide providers in ordering the most appropriate tests, procedures, and treatments for their members. This approach enhances patient care delivery and outcomes while improving provider relations and reducing healthcare treatment costs.
For example, a regional health plan was experiencing high prior authorization denial rates and provider dissatisfaction. The WNS Consult™ platform led to a demonstrated net direct savings ROI of 4.9, improved provider satisfaction and overall savings, and reduced prior authorization denial rates.
WNS’ model is proactive and focuses on behavior change rather than denial of services. It involves proactive outreach to ordering providers, offering clinical education with in-house clinicians, and modifying treatment plans to suit patients’ needs while reducing denials and abrasions.
It aims to continue to reform clinical guidance and authorization in two ways: a rigorous approach to clinical guideline development, and leveraging smart technology. At the same time, WNS offers a flexible approach to which activities it performs and which are retained in-house.
A Rigorous Approach to Clinical Guideline Development
Clinical knowledge is derived collaboratively and utilizes ~600 clinicians while promoting proactive peer outreach and integration of practicing physicians. This ensures that clinical decision-making includes comprehensive medical knowledge and real-world practice, leading to the efficacy of healthcare plans.
The platform’s clinical guidelines are based on research across:
- Governmental quality and regulatory guidelines
- Specialty society guidelines
- Evidence-based literature.
The governance model uses an independent panel comprising WNS clinicians and subject matter experts who review and update guidelines quarterly across ~400 topics and seven specialties. This process ensures that the evidence-based guidelines reflect the latest medical research and regulatory standards. These guidelines are then translated into detailed business rules that guide the Consult platform’s clinical decision-making process with branching logic, if-then, and ‘re-direct’ (auto-approval) rules.
Streamlining Authorizations with the Consult Platform
The authorization process begins with an order request submitted by the ordering physician through various channels (e.g., phone, fax, web, EHR). It enters the Consult platform and into its regulatory rule engine, which deciphers the requests against business rules and clinical guidelines. If the rule criteria are not met, the request progresses through a three-tier assessment and review before a denial or authorization is granted:
- Tier 1 – Initial assessment conducted
- Tier 2 – Nurse review
- Tier 3 – Peer-to-peer review.
If an order reaches Tier 3, the peer-to-peer review determines the appropriate course of action, which can result in a major procedure change or withdrawal of the order request. At any of the tiers, notifications are sent to the ordering provider and member if authorization is granted. If a request is denied, WNS issues a denial letter and handles all administrative communications, including denial language.
The Consult platform supports EMR connectivity and API-based architecture to provide seamless integration with existing healthcare systems, facilitating real-time data exchange, and improving the responsiveness of healthcare services. The platform has achieved ~80% automation and ~70% portal adoption, demonstrating high efficiency and user engagement.
The application of predictive analytics and AI within Consult allows for more intelligent decision-making and enhances the ability to forecast patient care needs and outcomes more effectively.
Offering a Flexible Service Model
Recognizing the diverse needs of health plans, WNS offers both delegated and non-delegated models, allowing for flexible integration of their services according to the strategic goals of the health plan. These models range from handing over everything from case intake to appeal management to WNS (delegated model) to health plans opting for non-delegated models, keeping certain services in-house (such as medical necessity decision and appeal management).
Looking Ahead: Continuous Improvement and Expansion
The WNS future roadmap includes clinical and non-clinical investments. Clinical expansion includes increased coverage of genetic testing, oncology clinical pathways, and post-acute programs. The non-clinical expansion includes enhancing the platform’s capabilities to include order pattern intelligence, UMaaS, and enhanced member engagement.
WNS’ initiatives will continue to offer improvements in how healthcare services are managed and delivered, leading to better outcomes for all stakeholders.
]]>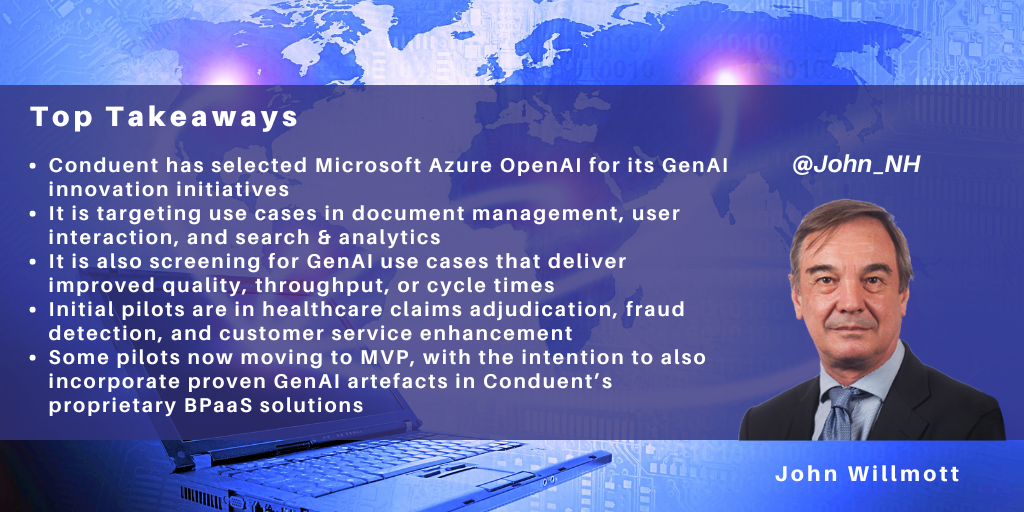
Conduent has partnered with Microsoft to use Microsoft Azure OpenAI to underpin its GenAI innovation initiatives with clients.
Its GenAI journey includes:
- Selecting use cases focused on improving quality, throughput, and cycle times
- Adoption of pilots in healthcare claims adjudication, fraud detection, and customer service enhancement
- Subsequently, moving to MVPs and industrializing use cases.
Use Case Selection Criteria Focused on Improving Quality, Throughput, and Cycle Times
Conduent recognizes that GenAI is an expensive technology and that its adoption will typically incur costs in changing existing processes and technology stacks. This makes it difficult to build GenAI business cases on already optimized operations based solely on cost reduction. Hence, Conduent is focusing on “innovative additive opportunities” to make the business case work.
The outcomes that Conduent is targeting from GenAI initiatives are:
- Improved quality, reducing error rates across standardized workflows
- Increased throughput of business process transactions
- Faster cycle times by consolidating value chain steps for faster processing.
At the same time, Conduent’s client relationships tend to involve relatively deep end-to-end service provision across a range of processes rather than single-process support. These combinations of services are tailored for specific clients rather than being standalone commoditized services.
Accordingly, Conduent’s document management services and CX services are generally supplied as part of a wider capability rather than as standalone services. Within this pattern, most of its solutions include elements of:
- Document management, including summarization & analysis, and extracting and contextualizing text within images
- User interaction/call center with multiple clients across various sectors, including enhancing agent assist, virtual agent, and call center agent assessment
- Search & analytics.
These three areas are regarded as core competencies by Conduent and all its GenAI use cases for the immediate future will fall into one of these areas and will be capable of delivering improved quality, throughput, and cycle times.
Initial GenAI PoCs Focus on Healthcare Claims Adjudication, Fraud Detection, and Customer Service Enhancement
Conduent has announced three GenAI pilot areas covering healthcare claims adjudication, state government program fraud detection, and customer service enhancement.
Conduent is a major provider of healthcare claims adjudication services. Here, it is working on a PoC with several healthcare clients to apply GenAI to reduce the error rate in data extraction and achieve faster cycle times in claims adjudication. GenAI is being used within document management to summarize highly unstructured documents, such as appeals documents and medical records, using its contextualization capabilities, including image-to-text. The technologies used are Azure AI Document Intelligence and Azure OpenAI Service.
Secondly, Conduent is working on a fraud detection PoC to support social programs in the U.S. state government sector. This PoC uses GenAI for search & analytics across multiple structured and unstructured data sets to increase the volume and speed of fraud detection. The technologies used here are Azure Data Factory and Azure OpenAI Service.
Finally, Conduent is using GenAI to enhance the use of agent assist and virtual agents by training virtual agents on existing data so that they can be deployed much faster.
Moving to MVPs and Industrializing GenAI Use Cases
Conduent initially undertook PoCs in the above areas to get both Conduent and the client comfortable with the results of applying GenAI and prove the use case. The PoC process is iterative and very granular, and Conduent perceives that organizations need to be extremely prescriptive to get the right results. This typically means defining the specific inputs and outputs of the use case very tightly, including defining what GenAI should do in the absence of individual inputs.
Conduent is now moving towards MVP and building client business cases in several of these pilots, including in some pilots in the document management space. Since Conduent has taken a horizontal approach to its use case selection, many of these have the potential to scale across multiple industry segments and clients.
In addition, Conduent provides BPaaS services to many of its clients, so it is looking to embed proven GenAI use cases in its proprietary technology platforms.
Existing use cases are business unit-sponsored but curated centrally, with the center providing enablement and cross-pollination across business units. However, the intention is to incubate future GenAI capability within individual business units.
]]>
In 2020, the U.S. healthcare payer BPS market saw accelerated growth in the adoption and design of digital solutions across all functional areas. The acceleration is driven mainly by consumer demand for an "Amazon" experience from their health plans and providers, to know the cost of care for associated benefit plans to assist in plan selection or inform decisions about elective procedures and treatments. It is also driven by approaching federal regulation deadlines. Specifically, regulatory requirements from the Cares Act and subsequent rulings from CMS are driving further steps towards interoperability throughout 2021-2024. These requirements follow the initiatives by CMS offering price lookup tools for outpatient procedures and OOP costs for physician visits for Medicare consumers.
Regulatory deadlines drive digital adoption
By January 1, 2022, private payers and group plans must standardize data files to be made publicly available and shared through APIs. The available data will be an opportunity for insurtechs and technology vendors to develop price comparison tools further and price analyses to inform their development.
After January 1, 2023, these payers must offer online plan comparison tools for consumers to view negotiated provider rates and personalized OOP costs estimations for 500 commonly utilized services. This will require real-time underwriting and price aggregation and analysis, with the ability to segment the data by facility and provider. Then, starting on January 1, 2024, individual and group plan consumers will be able to view the estimation of the total OOP costs, including usual tests, procedures, DME, and other items associated with specific treatment plans.
Opportunities for tech vendors to provide services & digital solutions
Without significant digital transformation, meeting the interoperability and price transparency requirements poses a considerable challenge for U.S. healthcare payers. Legacy and "home-grown" systems perpetuate siloed digital solutions, unstandardized data, and difficulties in designing APIs and intake of external data. The disjointed process becomes even more complicated when payers face these challenges on a seasonal basis to perform market assessments, develop products, and price new and renewed plans.
Additionally, payers face the challenge of complying with continual changes in required API formats, currently defined by HL7's FHIR. Payers will need support in converting or implementing the standard format and subsequent testing as regulations and required formats change, such as federal exchange marketplace plans that must implement FHIR APIs with third-party apps for open data access.
Capgemini spotlight: price transparency offerings
U.S. healthcare payers can obtain digital solutions to support regulatory compliance with Capgemini's price transparency solutions. Capgemini has 15 years of experience in the Medicare Advantage space, providing enrollment and member account maintenance management services, solutions, and advisory support. The recent focus has been on designing analytic and AI-driven tools for healthcare payer and provider clients in meeting regulatory guidelines and customer-driven demands for enhanced digital experiences and upfront cost estimations.
Capgemini offers service-line driven pricing for the average cost of medical care from hospitals and healthcare providers in the consumer's area. Capgemini developed the relative pricing guidance for hospitals, with an average of 1200 parameters per hospital for ~700 hospitals, categorizing both operational and overall spend by diagnosis parameters. The hospitals were then ranked into low, medium, high. In addition to overall price analysis, Capgemini parsed hospital spend by service line to provide cost estimations by diagnosis or treatment.
Capgemini is also working with several Blues to estimate OOP cost projections viewable on the member portal. Capgemini designed a cost calculator for a medical procedure at a specific healthcare facility, including the member's expected copay/deductible. A pricing engine was then implemented into a Blue's member portal to provide hyper-personalization, utilizing both internally available eligibility data and the aggregated market data for variable cost pricing. Currently, Capgemini offers implementations of ranking engines enabled by pricing algorithms and provider registries, returning search results of the top 10 providers most relevant for a specific diagnosis or procedure and the estimated cost of copay/deductible/OOP for each provider.
Capgemini's price transparency work is also heavily focused on utilizing MLR for cost-sharing estimations, including telehealth in the cost estimations. For a U.K. health plan, Capgemini implemented a solution to perform plan comparisons against industry standards, such as a specific member with a particular set of demographics and health characteristics, to estimate the eligibility and cost-sharing – competitive pricing. The solution incorporated several analytics tools to perform analysis and reporting on historical cost-sharing.
By the end of 2021, Capgemini's digital solutions in price transparency will integrate the payers' provider search tools to rank relevant providers based on health outcome metrics. Capgemini continues working with certain Blues plans to develop a marketplace with shared data and real-time quoting for care pricing and plan comparisons, involving interoperability and price transparency initiatives to benchmark the cost of services by area and plan. Additionally, Capgemini's development is focused on creating bundled pricing for all procedures and tests associated with a long-term treatment plan, as will be required of healthcare payers by 2024.
Increased demand and opportunities for digital transformation in the near future
The challenges faced by U.S. healthcare private and group payers present opportunities for technology vendors to provide digital solutions and services for payers to meet both the regulatory requirements and consumers' digital experience expectations. Client engagement types will vary by payer size, as many large payers only require specific solution design and implementation within their existing systems, while many mid-market and regional plans will be looking for BPaaS models of engagement with technology vendors. Payers will be looking for digital solutions to provide personalized real-time quotes for procedures and later for bundled pricing by the treatment plan and expanded data sharing to enable price transparency initiatives.
]]>
Digital front doors and transparency a new normal for healthcare?
U.S. healthcare is no stranger to an environment of continuous change and has not been spared the effects of the COVID-19 global pandemic in 2020. The unique circumstances born from the need for social distancing during the pandemic have accelerated healthcare consumers' demands for digital transformation. The ask comes from all healthcare continuum vantage points – patients, providers, payers, and vendors. Healthcare must change its practices to allow for more seamless digital interactions to meet these demands.
As with other service industry sectors, healthcare consumers want the option to access their health services virtually – evidenced by an increase from an 11% utilization of virtual visits in 2019 to over 45% in 2020. Some larger health systems have made this transition without significant challenges, expanding telehealth contracts, and receiving service reimbursements for both commercial and federally funded insurance types. However, many providers were faced with the decision to either suspend their practice or invest in digital platforms or services to offer virtual visits. Cognizant's Core Admin Solutions support providers' internal processes to offer telehealth and payers and providers in efficiently & quickly submitting process associated claims and authorizations via Trizetto's Touchless Authorization Processing (TTAP). The demand for telehealth has become an independent demand from the initial catalyst of social isolation and continues to be at the forefront of patient expectations. Even the senior population is thought to have few barriers to accessing virtual care, with 84% of sampled senior consumers stating they do not have any technical challenges in attending a virtual appointment with their doctor. With the remote operation of the doctor's visit comes the corresponding demand for total digital transformation; payment processing, e-prescription writing, prescription home delivery, and remote patient monitoring. Multi-faceted companies, like Cognizant, offer a variety of bundled or unbundled services and platforms to help healthcare providers and payers address the increased demands for digital interactions. This new digitization is also thought to reduce costs by increasing care coordination, administration, and manufacturing efficiency.
Providers and Payers are finding that digital products also offer the opportunity to clinically manage their patients and members remotely, with IoT, remote monitoring devices, and health wearables. The consumer can utilize various devices, measuring vitals, health coaching through AI, and tracking other metrics related to health risk factors. 65% of consumers utilize some type of wearable. With this percentage of adoption and available data, providers and payers have an exciting opportunity to address their patients' and members' health outside of the doctor's office. Vendors offer bundled platforms or paired digital services to collect, aggregate, and analyze the patient/member data to facilitate care management efforts by both their clinicians and their health plans. Though this digitization also requires a financial investment from the organizations, the vendors promise a visible ROI in cost savings and improved health outcomes.
Driving the transformation
Regulatory bodies have been pushing healthcare providers and payers towards a digital transformation, most recently with the ONC Cure's Act Final Rule. The rule was created to increase interoperability and access to consumer's own health information. Though the rule pushes providers and payers towards the shared goal of an enhanced patient experience, compliance with these requirements will come at a cost. By 2021 payers will be required to allow consumers access to all their claims and health information and to develop APIs to share data with other organizations and regulatory bodies. Though the compliance will be a financial investment for providers and payers, vendors such as Cognizant can implement or offer platforms to achieve such price transparency.
The Centers for Medicare and Medicaid Services (CMS) has similarly taken steps to guide providers and payers towards a better patient experience. In the 2021 Medicare Advantage Final Rule, CMS announced a change to its CMS Star Ratings measures, increasing the weight of the patient experience metrics. Payers must now invest more heavily in their consumer requirements – digital transformation to achieve an end-user-friendly suite of digital platforms. Cognizant addresses another of these drivers by offering several applications and platforms that facilitate both back-end processes and consumer-facing platforms in assisting payers in meeting heightened digital demands from their consumers. Cognizant's continued investment in Trizetto products offers payers such an opportunity for an enhanced user experience with an automated enrollment platform. Such an offering would make a payer more attractive in the upcoming Medicare Advantage and ACA Marketplace OEP (open enrollment period).
Healthcare organizations are also feeling the pressure for change from InsurTech companies and their partnerships with healthcare providers. These initiatives are attracting members and patients with their omni-channel user interfaces and strategic focus on digital platforms and processes.
Product Suites to Achieve the New Normal
Amongst Cognizant's comprehensive suite of product offerings, their digital healthcare platforms and services support over 200 million lives in the U.S. Payers and providers alike have the option to select a la carte products or bundled services to meet the changing regulatory requirements and evolving demands of their consumer and patient bases. Cognizant continues to exact leadership and be forward-thinking in its current and planned digital transformation offerings and continued investment in Trizetto Healthcare Products ($100m):
- Core Payer and TPA admin solutions, for claims processing and management
- Payer-provider solutions, for facilitating contract pricing and modeling and payment administration. Cognizant has planned offerings for onboarding and credentialing
- Government and Quality Solutions, for enrollment and encounter data management, and support of quality rating measures and reporting. Cognizant is planning offerings for enhanced care coordination
- Care Solutions, for clinical and utilization management and value-based benefits. Cognizant is planning offerings for for automated authorization and referral management
- Data orchestration SoE solutions for data aggregation and engagement. Planned offerings include additional integration and analytics for interoperability.
While Cognizant, and other vendors, offer a wealth of products and platforms for health systems and payers, for many the financial investment required has been a barrier. But COVID-19 is having an impact, in spite of an estimated four-month loss of $202.6bn for hospitals and health systems in the U.S. Every U.S. health system recently interviewed by NelsonHall regarded digital transformation as more important as a result of COVID-19, with increased investments planned in SaaS and cloud infrastructure. Overall, hospitals & health systems in the U.S. have shortened their planning horizons to address short-term priorities and investments. One major healthcare system stated that their planning horizon was now weeks rather than years. The same reduction in planning horizon is also evident in healthcare payers, but here with a need for customer retention combined with a much stronger emphasis on cost control.
As is true in other sectors, the pandemic will likely increase the acceleration of digital transformation initiatives across healthcare, with a clear focus on achieving short-term results (rather than in years), producing very immediate improvements in both productivity and customer experience.
]]>
In this blog, I look at how NTT DATA worked with a large Blue Cross Blue Shield (BCBS) health insurance carrier to establish an enterprise governance structure for automation, and at the lessons learnt along the way.
Like many other large BCBS carriers, the company had piloted RPA initiatives, and from the somewhat frustrating results of these experiments, it had formed two conclusions:
- An IT department-driven center of excellence delivering bots will not achieve the full potential of automation
- Point solutions being driven within individual towers/business units are not scalable across the enterprise.
The company concluded that before it could proceed with its automation journey, it required an automation governance structure that aligned with the enterprise strategy. A business-driven (rather than IT-driven) deployment of RPA needed to coordinate the needs, requirements and deployment of RPA across the front, middle and back office functions, as well as shared and internal ancillary services.
The BCBS carrier hired a team from NTT DATA, led by Deana Rhoades, the Global Practice Lead, Healthcare Automation “to create an enterprise-wide governance structure customized to their corporate strategic objectives and organizational culture”. Within the context of the enterprise’s goals, strategy, and current workforce, the company tasked NTT DATA to create the automation strategy, the decision frameworks and the organizational structure. While the BCBS company had long before established solid objectives, frameworks and management systems for its human workforce, the company realized it needed to lay the foundation for the same kind of structure for automation (and the bots) of its “digital workforce”.
Starting in August of 2018, NTT DATA began its work creating an enterprise level governance structure for automation. It focused on scalability considerations and governance, treating bot development “almost as an afterthought”. The tactical view about how to purchase and deploy automation solutions and build bots on different platforms would flow from the enterprise’s strategic objectives and from appropriate integration of the human and the proposed digital workforces. It took two months for NTT DATA and its client to articulate the following governance model, composed of three layers:
Layer 1: Sponsorship
Champions of the RPA transformation articulated the vision and goals for the automation journey and monitored performance of the COE. Sponsors include high-level representatives of the COO, the CIO and the HR departments, coordinated by a Program Management Office (PMO). Strategic frameworks now articulate the enterprise’s objectives, categorize potential automation projects within that context, and facilitate decisions about deployment in terms of (for example):
- Potential cost savings (prioritized over revenue)
- User experience (prioritized over productivity).
Layer 2: Enterprise Capability Center
This team unites leaders and dedicated resources from the following functions: HR, Data and Analytics, IT, Security, Organizational Change Management, Business Process Management, and Operations. Six workgroups develop and provide expertise on the core COE capabilities. The COE subgroups cascade the automation strategy into action plans that provide capabilities across automation development teams and business units. Focus areas include:
- Strategy and Measurement – turns strategy into executable components; owns success criteria, key performance indicators (KPIs) and objectives and key results (OKRs); quantifies the value of the COE
- Pipeline Management – generates demand for automation at the process level among BCBS company employees, prioritizes and schedules the resulting workstreams
- Workforce Strategy – defines needed FTE skills and gaps, owns the organizational change management (OCM) plans and provides training for BCBS company employees
- Automation Standards – develops the standards, tools, repositories, policies and procedures that guide all automation initiatives
- Data Strategy – maintains data management strategy, defines how automation software accesses and collects data, and how the automation efforts comply with risk and security policies
- Virtual Workforce Monitoring – maintains a centralized command center to monitor and oversee the bots in production.
Layer 3: Automation Factory
Delivery and deployment teams work under the aegis of the leadership priorities and plans developed in layers 1 and 2 with complementary aims:
- Demand generation – generating awareness and demand for automation within the enterprise at the level of the teams that manage specific processes. A change management team trains these teams on capabilities of RPA and helps them see the value of implementing the technology
- Technology delivery – agile development teams automate processes using the appropriate tools and platforms, such as Blue Prism and UI Path.
For the next phase of work, NTT DATA has begun to create a complementary hybrid (or “federated”) operating model for agile delivery of bots. This hybrid model is supposed to establish the guardrails and frameworks needed by individual business units that have the skills and the desire to build their own bots. The hybrid model is expected to augment the centralized enterprise governance model by 2020.
The human response?
With NTT DATA, the BCBS company has worked to communicate with various business units and with their leaders to resolve their questions and any potential anxiety about the use of bots. During the BCBS company’s prior work with another IT consulting firm, it had developed its own home-grown automation tools. The in-house deployment of an RPA platform had introduced the company to concepts and practices at a tactical level. Activities surrounding these pilots had been widely broadcast through various communication channels, including robotic roadshows, Yammer, and email. As a result of this in-house publicity, NTT DATA reported that it met with more curiosity and less resistance than expected. NTT DATA also reported that company business units and employees had already begun to form opinions about automation through the lens of their experience with their prior RPA tool, opinions that needed to be considered if and when other development tools were introduced.
The business consequence?
NTT DATA believes that the BCBS carrier has taken a significant stride up the automation maturity curve by articulating a governance model with the following elements
- Charter
- Roles and responsibilities
- Leaders
- Change management
- Resources dedicated to organizational communication and demand generation
- Resources dedicated to development of a broader set of intelligent automation technologies.
RPA initiatives that predate the NTT DATA-led exercise in defining automation governance now have a structure and resources available when they need to escalate issues, and have realized greater ROI. Furthermore, the BCBS carrier’s “ox in the ditch” initiatives have now been organized into six workstreams, and in future the company believes that its governance structure and measured approach will yield expected ROI and that its human and virtual workforces will complement each other efficiently.
]]>
In my previous blog, I described how, since 2017, Sutherland has created a shared services model that obviates the need for participating California health plans to separately build and update parallel databases to track the availability of providers of nonurgent care for Medicaid recipients.
The company estimates that through its consortium of member health plans it has reduced associated health plan physician data management costs by 75% through elimination of duplicative work and by improvement in survey execution workflow and other areas. For an estimated 80,000 physicians in its CA directory, Sutherland now estimates that it reduces the touch rate on providers related to the Provider Appointment Availability Survey (PAAS) from three to one call per practice. The initiative also improves reporting and other interactions with the California regulatory body (Department of Managed Healthcare, or DMHC) and improves patient access to timely care.
Sutherland’s success with its coopetition/shared services model begs an interesting question: can this model be extended across the U.S. and, if so, how?
Uncovering value from duplicated effort
The coopetition model now proven in California might provide a useful template for future work at the national level. Data from Sutherland’s efforts in California indicate that national health plan provider networks significantly overlap and that much of the work they pursue in building and maintaining their physician databases is therefore duplicative and wasteful. In California, Sutherland reports a 48% overlap of providers between the top three CA health plans. That is, of ~20,000 physicians that are currently contracted to plans managed by one of the top three health plans in CA’s Medi-Cal Medicaid program, over 9,000 are currently contracted with all three health plans. Each health plan in California is required by the DMHC to maintain accurate data on each provider so that patients can gain access to timely care. Each health plan is further required to manage this dataset in order to maintain its own operations. The difficulties in maintaining these parallel datasets result in a myriad of problems for different stakeholders, including wasted effort.
Stakeholders include vendors of business outsourcing services. Prior to Sutherland’s involvement in the shared services initiative, the data collected by the DMHC was of such poor quality that it resulted in a directive to all CA health plans saying that the vendor then in charge of managing the provider data collection effort would no longer be allowed to work in CA.
Sutherland reported that, at that time, 40% of data records contained errors or omissions. The result was that health plans could not confirm members for timely and appropriate access to care, and providers were subjected to unnecessary inconvenience, cost and fatigue. The opportunity for a vendor of business outsourcing services, conversely, was significant. Since two-thirds of data collection efforts by different health plans required the same basic information from providers, Sutherland identified an opportunity in California to generate value by eliminating unnecessary work and collecting a slice of the resulting value, while simultaneously providing value to the regulatory body, providers, and patients.
Geographic & market segment extension of the model
The geographic extension of this model in physician network data management beyond California may be a logical next step. Sutherland itself calls its shared services model for the provider appointment availability survey (PAAS) a “proof of concept”. The fact that Sutherland has successfully united the interests of competing health plans with those of providers, patients, and the state regulatory body lends credence to the idea that other health plans in the U.S. might be convinced to join a similar consortium. Note that some health plans would likely never be candidates, such as Kaiser Permanente, which is based on a vertically integrated model that unifies the management of provision and reimbursement of care. (While Kaiser provides Medicaid services in California, it is not a member of Sutherland’s current shared services model in CA).
However, whether led by Sutherland or another entity (private or public sector), such a consortium could eliminate waste on a state-by-state basis, or even more broadly. The model could be extended to other government healthcare. It could standardize and streamline data collection, present accurate data to a wide range of stakeholders in timely fashion, standardize reporting, reduce provider fatigue significantly, and improve customer/patient access.
Generating leverage
Creating a public utility by mandate may lead to inefficient, unintended consequences, but Sutherland’s success seems to indicate that a market solution can be viable. The CA consortium currently counts 14 health plans, but replicating this success outside CA would require customization to other economic and political circumstances. The mission of the Council for Affordable Quality Healthcare (CAQH) and other associated alliances, non-profits, and government agencies may align with such efforts. Companies that specialize in providing outsourcing services have, as Sutherland proves, many of the capabilities required. Short of a government-sponsored mandate, how can health plans be induced to share proprietary data and data methodologies?
Political leverage might be hard to generate among consumers/patients, but physicians may present a more unified and sharply-focused interest group. If a doctor contracts with a single health plan for multiple products (e.g. Medicare Advantage, Mental Health, etc.) and that doctor’s information needs to be verified for each product, this would require multiple touches, cost, inconvenience, and fatigue. According to Sutherland’s experience in CA, that doctor may, on average, contract with 20 health plan products. The doctor is therefore incentivized to reduce this duplicative and wasteful interaction, and the argument that physician rosters can be harmonized among health plans with minimal interaction (leveraging web portals rather than call centers) is not hard to make. Having thus grasped the challenge, the physicians’ professional organizations may be well-placed to work with health plans to set up more consortia similar to Sutherland’s in California.
Finding allies
An industry alliance designed to introduce blockchain is aimed directly at the challenge of reducing the estimated $2.1 bn in cost associated with maintaining provider data. According to an April 2018 healthcareITnews.com article, Optum, UnitedHealthcare, Humana, others launch blockchain pilot, these industry titans are exploiting the opportunity to reduce waste associated with provider data: “Five healthcare organizations including insurers UnitedHealthcare and Humana, Optum, Quest Diagnostics and MultiPlan are launching a blockchain pilot to help payers tackle mandated provider directories”.
The mission of this alliance may provide a long-term objective to which one or more consortia based on the Sutherland CA model might be mutually supportive. The hype associated with blockchain might create the attention necessary to establish more provider data consortia, while the political clout of physicians’ professional organizations might bring leverage. In combination, private sector players might then find the resources and support necessary to align economic incentives, manage workflows, normalize and de-duplicate data, execute against state and federal regulations, and package provider data in digestible, accurate, up-to-date formats for the constellation of healthcare stakeholders.
]]>
Benefitfocus, the cloud-based benefits management platform and services provider, recently hosted 1,200 benefits professionals at their annual One Place conference in Charleston, S.C. The conference featured updates on Benefitfocus’ strategy, enterprise benefits management technology platform, and partners from its ecosystem; and presented an opportunity to learn from industry thought leaders, technology partners, benefits suppliers, and insurance brokers. On the final day of the event the company facilitated employer efforts to build benefit strategies and experiences at what was billed as the industry’s “largest open enrollment planning event”.
During the event, Benefitfocus updated customers and ecosystem partners on seven key topics, as covered in this blog.
Shift in corporate strategy
Benefitfocus has embarked on a significant strategic realignment. The company is shifting its company strategy from selling software to facilitating a benefits industry platform (or marketplace, such as Amazon). The company has been influenced by the book Platform Revolution, written by MIT professor Geoffrey Parker, who was introduced via a recorded video after having visited the company at its campus headquarters in South Carolina. Parker’s book instructs leaders how to start and run a successful platform business such as Amazon, explaining ways to identify prime markets and monetize networks.
Benefitfocus’ ambition is to “connect benefits buyers and sellers in unprecedented ways” and be accepted in a new bracket of peers, including Amazon, airbnb, and Uber. In practical terms, newly introduced analytics are designed to allow sellers and brokers using Benefitfocus’ SaaS software to segment employer customers and employee populations for “improved benefit strategy, communications and engagement, while giving employers robust visual interactive tools to quantify the value of their benefits programs and serve their employees.”
However, questions regarding the practical ramifications of this strategic shift remained unaddressed in the general sessions, including:
- The shift from a software development culture habituated to a standard, planned software roadmap and update release schedule to a “platform” culture habituated to agile development
- Adaptation of the Benefitfocus sales channel, sales methodology, sales collateral, sales and marketing resource roles, responsibilities and staffing
- Development of an ecosystem partnership within a complex web of coopetition (in which medical carriers, for example, may currently go to market on the Benefitfocus SaaS software, white label Benefitfocus, and/or go to market concurrently with their own home-grown development platforms).
- Development of the benefits administration professional community within Benefitfocus’ ecosystem of employers, consumers, and benefit providers.
Software updates
Benefitfocus platform updates that resonated strongly with benefits partners included:
- Mobile App: It is now possible to email or text health data to a physician, including proof of insurance. This is a service not only for the consumer but for the insurance carrier that wants to have accurate data conveyed to physicians in real-time. The Mobile App aims to simplify consumer engagement, total rewards details, and digital ID cards. Enrollment can now be accomplished using the Mobile App.
- Chatbot: Embedded in AI engine BenefitSAIGE, this 24-hour chatbot drives content and recommendations to consumers every type of benefit at every stage of life. It also frees the HR professional who is ordinarily called to interface with consumers about the benefits platform and benefits companies. Chatbot communications limit delays generated by hand-offs as a consumer inquiry passes to the HR professional, to a benefits broker, to a benefits vendor, and then returns back to the HR professional and finally the consumer. The chatbot also drives appropriate benefits enrollment in “smart moments” that matter to consumers.
- Digital Wallet: This feature enables flexible payment options beyond payroll deduction. Payment using personal credit cards can also be accomplished using the Mobile App. The platform now allows employees to purchase insurance at any time during the year, not just during a two-week open enrollment period.
Other notable added software functionality includes:
- Data interchange and automation enhancements, analytics and communications enabled by AI engine BenefitSAIGE. The AI engine leverages rules-based systems, RPA, machine learning, predictive analytics, and natural language processing. This AI engine aims to improve data interchange, drive insights, improve the consumer experience, and influence transactions during “smart moments”
- Ecosystem productivity enhancements via data exchange, APIs and automation, supported by security and data protection.
Benefitfocus reports that over 25m consumers are now served by its software platform. Clients include 170k+ employers, from Fortune 500 companies to small employers, featuring 17k brokers, 144 medical benefits carriers, and 30+ marquee voluntary and specialty benefit brands.
Data cleansing
The company reports that a $30m investment has produced a dataset with “99.6% data accuracy on first-pass yield, eclipsing the industry average of 95%”. The dataset includes records of 2.7bn data transactions in 2018 alone.
Adding a portable life insurance partner
BenefitsPlace now features Afficiency, an InsurTech that is working with life insurance carriers to offer portable voluntary life insurance benefits.
Adding consumer-directed health partners
The company has also added greater choice of consumer-directed healthcare (CDH) account options, including Wageworks and Payflex. API connections are designed for synchronized, accurate and real-time data exchange. Year-round education and communications should help consumers maximize their CDH contributions, including the triple-tax benefits of funding their HSAs.
Introduction of personal lines insurance products
On the existing software platform, insurance carriers and specialty product suppliers gain a dedicated digital distribution and enrollment channel to more than 23m consumers on the Benefitfocus platform. Carriers included in this first iteration include:
- Bristol West Insurance Group: a member of the Farmers Insurance Group of Companies (PL auto)
- MetLife Auto & Home: Metropolitan Property and Casualty Insurance Company and its subsidiaries, operating collectively under the MetLife Auto & Home brand (PL auto and homeowner)
- Toggle: launched by Farmers Insurance in 2018 (renter’s insurance).
Benefitfocus offers P&C insurance through licensed brokers at discounted rates.
Innovation incubator
Benefitfocus announced its InnovationPlace, a startup partner program. The company aims to introduce innovative products and services to employers and their employees through its SaaS facilitated marketplace. The company has created an innovation incubator on the company’s South Carolina campus, and welcomed its first occupant, Rock Health, an innovator in women’s health.
]]>
In this blog, I look at how Sutherland tackled the challenge of health plans maintaining accurate provider data in the state of California.
The challenge: inaccurate health plan data about providers
It’s been difficult for health plans in California to maintain accurate, up-to-date information on the current status of providers in the state. According to outsourcing vendor Sutherland, experience indicates that 60% of provider directories contain serious material errors. Health plan data frequently indicated that doctors were no longer accepting new patients, even though they in fact were. The data frequently presented the state regulatory body, health plans, and patients with inaccurate information about whether doctors continued to practice their specialty, had moved to new locations, or were contracted to work with particular health plans or their products.
The context: gaining access to timely CA medical services
Since 2017, Sutherland has created a shared services model for over a dozen CA health plans that obviates the need for participating California health plans to each separately build and update parallel databases that track the availability of provider appointments for urgent and non-urgent care for health plan members. The State Department of Managed Healthcare (DMHC), which regulates the state’s health plans, requires that health plans and providers make available appointments for urgent and non-urgent care, varying by specialty, from two to 14 days. Until recently, each health plan created and updated its own massive database of providers that participated in each of those plan’s products.
In a state in which Sutherland reports that the average provider contracts with ~ 15 health plan products, the law resulted in a myriad of duplicative efforts, each of which imposed burdensome requirements on providers.
The Sutherland solution
Sutherland has initiated a shared services platform that reduces this burden for health plans, providers, and state agencies, and increases the accuracy of reporting to the DMHC. In particular, Sutherland spearheaded the coopetition of health plans in California in 2017 by creating a shared services model that built and updated the Provider Appointment Availability Survey (PAAS) on behalf of a consortium.
Prior to that, Sutherland had been in conversations with the state of California on a related topic, and that conversation helped initiate Sutherland’s PAAS project with the state. Sutherland had already built a relationship with Blue Shield of CA, which became the anchor client. Other state-based and national health plans joined the consortium in 2017, totaling eight by the end of 2017. By the end of 2018, 12 health plans had joined the consortium and Sutherland now counts that consortium at 14 health plans.
Sutherland estimates that it now touches ~ 100K doctors, each of which has contracts with an average of two plans. This hub-and-spoke shared services model eliminates duplicate outreach to CA providers, saving each participating health plan from the costs of maintaining separate call center facilities and databases, and saving providers from responding to multiplicative health plan outreach regarding the same basic data. Sutherland also manages all the workflows involved with credentialing a new provider, verifying diplomas, board certifications, and combing regulatory authorities for any information on sanctions against providers.
The company estimates that it reduced associated health plan physician data management costs by 75% through elimination of duplicative work and by improvement in survey execution workflow and other improvements. Sutherland estimates that it reduces the touches on providers from 3 to 1 call per practice, improves reporting and other interactions with the California regulatory body, and improves patient access to timely care.
]]>
The challenge of rising healthcare costs in the U.S. has been obvious for decades. Or has it? Various interventions have been attempted, but health costs as a percentage of GDP are forecast to continue to climb. National U.S. healthcare expenditure as a percentage of GDP has risen from 17.2% in 2011 to 17.9% in 2017.
In February 2018, the U.S. CMS Office of the Actuary estimated that “growth in national health spending is projected to be faster than projected growth in GDP by 1.0 percentage point over 2017-2026. As a result, the report projects the health share of GDP to rise from 17.9 percent in 2016 to 19.7 percent by 2026.” GDP growth over the last two periods has kept pace with rising healthcare costs over the last two years, but when GDP growth subsides, the healthcare cost challenge will reemerge. The current stalemate at the U.S. federal level about the path forward for healthcare reflects a lack of consensus about root causes and, therefore, advisable policy.
The sector has already undergone major restructuring and intervention, both government and private sector initiatives. This includes:
- The American Recovery and Reinvestment Act of 2009 (ARRA) incentivized adoption of EHRs – the assumption was that a lack of electronic clinical records technology was a primary component of inefficiency and waste. 90%+ of U.S. hospitals have now adopted EHR technology
- The Accountable Care Act (ACA) of 2010 realigned much of American healthcare reimbursement and delivery – the assumption was that decentralized, misaligned organizations created waste and reduced quality. The ACA introduced a raft of initiatives designed to address waste and improve productivity, particularly clinical labor productivity. The results of most of these measures, including the ACA’s Accountable Care Organization initiatives (ACOs) remain inconclusive
- Consolidation: the payer and provider markets have been roiled by restructuring and consolidation. There were 1,412 hospital mergers between 1998 and 2015; physicians also have consolidated into increasingly larger groups. Moreover, the four largest insurers now account for 83 % of the total national market.” [1].
The largest target for improvement in healthcare delivery costs remains the cost of labor. But does more “technology” improve labor productivity? Not necessarily. Technology can drive rather than retard growth in healthcare costs. According to a Health Affairs (HA) article, “technological changes in the [physician and nursing] sector to date have favored, rather than substituted for, those with high skills" [2]. It depends on the type of work or process, on the technology use case, and on the organizational aptitude for adopting new solutions. Administration, management and IT are oft-cited as a source of burgeoning healthcare delivery costs, but these classes of labor may actually be seen as examples to be followed. Over the 15-year period of the HA study, compensation (change in employment x change in earnings) for administration, management and IT rose only 35.3%. Over the same period, compensation for physicians and nurses rose 80.5%.
Taking a step back, have all the industry-level efforts at restructuring mentioned above missed the mark? Have we simply failed to appreciate how unhealthy Americans have become – and therefore overlooked the root cause of precipitous cost increases? The debates and struggles regarding GDP growth, healthcare delivery cost growth, technology adoption, government intervention, and market restructuring may simply be addressing symptoms rather than causes of the rise in U.S. healthcare costs.
The “hidden in plain sight” fact may be that Americans have unhealthy habits which have national ramifications for healthcare costs. In one 2013 study, only 2.7% of the U.S. adult population could be identified with healthy metrics for exercise, diet, smoking, and body fat. As national healthcare expenditures rise towards 20% of GDP, perhaps we should ask whether the challenge of rising healthcare costs can be adequately addressed by industry-level restructuring efforts. Perhaps this challenge can better be addressed by bottom-up rather than top-down initiatives.
[1] The Commonwealth Fund, Insurer Market Power Lowers Prices in Numerous Concentrated Provider Markets, September 6, 2017
[2] Where the Money Goes: The Evolving Expenses of the US Healthcare System, Health Affairs, July 2016

The insurance outsourcing industry is moving at a fast pace in response to the need for rapid deployment of digital platforms and offerings, as well as advancements in new distribution models that are emerging via ‘insurtech’ start-ups. Here I take a look at some of the key trends driving the insurance BPS market in 2017, both in terms of delivery and transformation, and by individual service line.
New distribution models, analytics & automation
Health insurance start-ups (Oscar Health, Clover Health, Bright Health, etc.) have been flourishing, followed by property & casualty insurance (Lemonade, Verifly, Metromile, Wrisk, etc.) and life & annuities insurance (Ladder, League, InforcePro, etc.), who are also seeing an increasing amount of investment. Outsourcing vendors will be actively looking to partner with, or potentially acquire, such companies in order to leverage their capabilities on an add-on basis, or using a completely transformative approach. And the insurance start-ups that will be most targeted by vendors are those investing in new distribution models.
Insurtech developments will bring more regulations at federal level in the U.S., as the application of new operational models will overtake the current state-level regulation framework of insurance companies. It is also possible that the new regulations will allow for the fostering of further innovation compared to current state regulatory frameworks.
Big data and analytics in insurance will see further growth, stemming from the vast amounts of data stored by insurance carriers. Vendors will either develop offerings to leverage such information, or will acquire companies in order to do so. It is still commonplace to find old-school insurers who are unable to analyze and leverage their clients’ and prospective clients’ data.
In terms of operating systems, vendors will continue to optimize legacy platforms with add-on proprietary or third party software, as well as retire dysfunctional and costly systems for newer ones that have modern distribution model capabilities. Digital transformation will increase among insurers, with larger numbers of insurance carriers shifting their operational model towards emerging market segments (millennials, middle-market consumers, etc.).
In the area of automation, the insurance sector has been at the forefront of RPA adoption to date, and this will continue in 2017. Meanwhile, AI technology is taking small steps towards greater adoption within insurance offerings, mostly in policyholder-facing applications. Policyholders will continue to request better, more personalized, engagement by their carriers through omni-channels, with a digital approach, with the policyholder engagement market segment seeing growth of more than 10% per annum.
Elsewhere, wider application of telematics offerings among passenger vehicles and industrial devices will allow for more accurate and individualized calculation of premiums.
Trends for 2017 by insurance service line
Property & Casualty BPS trends include:
- Launching new digital products and services in untapped markets for traditional insurers
- Emergence of fully digitally-operating carriers with a Bermuda-style regulatory framework, backed by PE/VC firms
- Emergence of new products for traditional insurers (drone insurance, on demand insurance, etc.)
- Wider application of analytics for process improvement and trend identification among policyholders.
Life & Annuity BPS trends include:
- Insurers outsourcing more responsibility to vendors that are able to provide specialized actuarial and predictive analytics services targeting customer retention
- Insurers requiring guidance on regulatory product adjustment from Solvency II implementations
- The middle-income and millennials market in the U.S. will see increased growth, as investments in digital channel communications expand
- Vendors will continue to improve customer service levels, CSAT scores and customer retention rates.
Healthcare Payer BPS trends include:
- The future of Obamacare and health insurance exchanges in the U.S. is uncertain after the Trump election. There will definitely be changes in the ACA care models and payers will most probably bear some of this cost of change in healthcare policy
- Consolidation among lower-tier healthcare payers will continue its momentum in 2017, creating opportunities for legacy platform retirements and updates from outsourcing vendors, eliminating disparate assets in newly-formed organizations
- Population health management and wellness programs through innovative delivery and distribution models will see significant growth, as well as engaging with patients through omni-channels, improving retention and satisfaction
- Applying analytics that identify opportunities for process improvement, as well as reducing fraud, waste, and abuse will be a top priority for payers
- Distant monitoring of patients and telemedicine will also see increased growth
- Preventive care and wellness offerings, in conjunction with traditional healthcare insurance, will see a rise in demand.
We now turn our attention to Dell Services, which has adopted an automation focus across its life and healthcare insurance BPS processes.
Focusing on healthcare payer & provider and life insurance process automation
In 2016, life insurance accounts for around 30% of Dell Services’ overall BPS revenues and healthcare payer accounts for approximately 35%, with healthcare provider making up the balance. Dell Services takes a platform-led approach to its BPS:
-
It has its own LifeSys platform for life insurance, on to which it migrates a client’s book of business and provides administration services in its own environment; or
-
It partners with a third party supplier for platform capability and tailors it to fit the needs of the book of business, from which it can then provide services, e.g. Dell Services uses partner ikaSystems for its healthcare payer platform needs, on top of which it layers its Dell Business Process Management Suite (DBPMS) tools. The tools include:
-
An enterprise dashboard: including KPI tracking and trend analysis for SLA metrics
-
Client extranet: including an issues log
-
Queue management: including skill-set based routing and priority allocation.
Automation Ideation led by BPS delivery teams
Unlike other providers, who tend to be led by their clients with respect to automation, the process at Dell Services starts with an internal ‘ideas generation’ stage, achieved either through Dell’s ‘LEAP’ (Listen, Engage, Act, Progress) portal where agents are able to log ideas, together with perceived benefits (and are rewarded if their ideas are selected) or via the Business Process Improvement (BPI) team who carry out a ‘click study’ to identify ways in which the process could be re-engineered or automated. In line with its peers, an internal concern about increasing automation was the inevitable change in job composition; for this reason, the LEAP portal is considered particularly important to ensure employees are involved and engaged in driving the initiative forward. In addition, supervisors are targeted with an annual 5%-15% AFTE target. Once an idea has been selected, a feasibility study takes place before the idea is tested and bots are deployed by the central AFTE automation team. Bot management is then passed to the operations team while the bots are monitored through the central bot command center.
Balancing AFTEs with FTEs
In line with the market, Dell Services has concentrated its efforts on applying automation to high volume processes, which account for ~30% to 35% of its overall book of business. To achieve this, it is targeting the introduction of ~300-400 AFTEs year on year, though this is not a static number since clients are on-boarded throughout the year. The overall aim is to achieve around 6% productivity improvement per annum.
Although Dell Services does use third-party RPA platforms, it has developed its own “AFTE” platform incorporated within the Dell Business Process Management Platform. AFTE bots rather than third-party bots are typically deployed where the Dell BPMS platform is already being used or is to be used.
High volume processes (in which AFTEs are being used to varying extents) within each of Dell Services’ insurance services include:
- Life insurance:
- Data entry and indexing: freeing up FTEs to carry out other activities such as policy holder services where less work is typically carried out by AFTEs – though this is something that Dell is looking to change and where Dell is investing in automation initiatives
- Policy issuing: currently, the work is handled 50% by FTEs and 50% by AFTEs, with Dell seeking greater tool maturity before it is able to drive greater automation here
- Premium accounting
- Healthcare payer:
- In-bound calls: FTE-led
- Adjustments: FTE-led
- Adjudication: 50% AFTE, 50% FTE
- Claim processing: FTE-led
- Member enrolment: FTE-led
- Provider maintenance: 50% AFTE, 50% FTE
- Healthcare provider:
- File download: exclusively AFTE
- Medical coding: 50% AFTE, 50% FTE
- Change entry: FTE-led
- Payment posting: AFTE-led
- Credit balancing: 50% AFTE, 50% FTE
- Accounts receivables: FTE-led
A simple example to illustrate some of the quantifiable benefits that have been achieved through automation can be seen through the work that took place to automate call center operations at one of Dell’s life insurance clients. Prior to the introduction of automation, call center agents were required to use a number of screens to capture customer information, which often resulted in comparatively low accuracy, and a high handling time. The system was not user-friendly and baseline training typically took around 10 weeks. Ultimately SLAs were being missed. To address this, Dell condensed the numerous screens into one screen and introduced rule-based processes to ensure no manual calculations were required to complete the form, unlike previously, where up to six manual calculations were required. As a result, AHT fell from 471 seconds to 374 and training took ~7 weeks, as opposed to 10. The quality of data capture increased from 88% to 95% and the average time taken to update notes fell from 110 seconds to 15 seconds¸ because the system was largely able to perform updates itself.
Plans to Implement Machine Learning within Dell BPM Platform
Over the last four years, Dell has extended its capabilities from simple script based-processing, to the development of AFTEs, including an associated AFTE command center. Going forward, the intention is to incorporate a self-learning capability, implement technologies such as NLP and machine learning within the Dell BPMS platform, and to secure end-to-end automation in the processes that are already largely being carried out by AFTEs, e.g. indexing.
]]>HPS' 2015 revenues were $223m. It has achieved a CAAGR of 38% in the last three years, driven both from adding new healthcare payers and from the increase in individuals or groups eligible for first-time insurance coverage due to the ACA initiations; the company now supports ~20% of Individual health plans in the U.S.
The acquisition will be a major boost to Wipro’s ambitions in healthcare and specifically healthcare payer BPS, an area where the company had made modest at best progress since its acquisition of Infocrossing, and the Infocrossing Healthcare Services, Inc. unit in 2007. Wipro Infocrossing currently has healthcare payer BPS contracts with two State Medicaid agencies, including Missouri’s Department of Social Services.
The acquisition of HPS will enable Wipro to move beyond support for the Over 65 market in the form of Medicaid and Medicare, and to address the growing market for individual plans in the Under 65 B2C market. It will provide Wipro with a more modern building block around which to position its healthcare payer BPS business. Such is the importance attached to this building block by Wipro that it is conducting a reverse integration of its healthcare & life sciences business into HPS, with the overall unit being led by HPS' President and CEO Jeff W. Bak.
The Individual policy market is currently a small part of the overall health plan policy base, but it is one that has been showing double-digit growth with the ongoing extension of health insurance coverage in the U.S. Looking at the future dynamics of this market, Wipro expects that the Individual plan member base will continue to grow for the next three years as health insurance coverage of the population continues to expand and will then stabilize. By this point, Wipro perceives that there will be a secondary growth driver for exchanges with health insurance exchange markets becoming attractive to employers as a mechanism for providing health plans to certain groups of employees such as part-time staff.
HPS currently serves ~35 healthcare payers, with its top ten clients accounting for ~80% of its revenues. Its client list includes Ameritas, Allstate, Assurant Health, Beazley, Cigna, Foresters, Humana, Kaiser Permanente, Starmark, UnitedHealthOne, unum, and vsp. HPS’ niche is in assisting healthcare payers to enter and control their costs around state-based and Federal exchanges; it is focused on the ‘individual’/B2C health plan market. HPS has a platform to support healthcare payers across the Individual policy lifecycle and views the typical journey with a healthcare payer in four steps:
- Helping them to connect with private & public exchanges (using its ExchangeLink platform)
- Assisting them in policy administration & member services (ServiceLink platform)
- Helping them with member acquisition through its licensed agents (SalesLink)
- Assisting them in member retention & loyalty (LoyaltyLink).
With these services, HPS can connect healthcare payers to 40 public exchanges and 150 private health insurance exchanges; and the HPS Insurance Agency connects to a network of ~100k nsurance agents. HPS aims to help payers move beyond medical insurance and offer servicing around digital products in other areas such as dental insurance and even life insurance.
HPS has ~2k employees, all onshore U.S. It offers both SaaS and BPaaS services. Clearly the BPaaS element is extremely attractive to Wipro and in line with its strategy for developing its BPS service. HPS will also give Wipro access to a wider client base among commercial healthcare payers and an opportunity to cross-sell wider services such as offshore-centric claims processing while adding credibility to the company’s onshore presence in the U.S. The non-FTE pricing models used by HPS (such as per member per month for member servicing and on a share of premium/commission for new business) will also be attractive to Wipro
Overall, this acquisition will give Wipro both a leadership position in BPS in the Individual healthcare payer market and also the potential for a fresh start in healthcare payer BPS overall, including opportunities to leverage its services around digital and analytics and to start to move into complementary areas such as population health management, patient monitoring, and ACO support. Possible synergies with other analytics offerings should not be excluded, such as with Wipro’s Marvel CX, in order to further enhance customer experience.
Wipro is on a bit of an acquisition spree at the moment: this will be its fourth acquisition so far in FY 16, following those of:
- Designit, which has enhanced the capabilities of Wipro Digital (part of the Change strategy)
- cellent AG, bringing in scale and local relationships in the key European market of Germany
- Viteos Group, bring in BPaaS capabilities in the financial services sector.
Including HPS, Wipro will be making an overall investment of ~$750m in these acquisitions, all of which are strategic, rather than bolt-on, acquisitions. Like Viteos, HPS will afford Wipro the opportunity to build a BPaaS business in one of its principal target sectors.
Footnote: NelsonHall prediction was spot on!
In our January blog on the announcement of the appointment of Abid Neemuchwala as the new Wipro CEO (see here), we said an acquisition like this was highly likely. And in our December 2015 Key Vendor Assessment on Wipro (which will be updated later this week) NelsonHall anticipated that the acquisition spree in FY16 was not finished with Viteos.
If you would like to know more about NelsonHall's extensive coverage of Wipro in our Key Vendor Assessment or any of our IT Services or BPS programs, please contact [email protected]
]]>TriZetto has a headcount of 3.7k (Cognizant at end of H1 2014: 187k.4). In its last 12 months, TriZetto had $711m in revenues and a non-GAAP operating margin of 18.4% (Cognizant in 2013: 20.6%).
TriZetto LTM revenues breakdown by service/product line is:
- Payer software: 40% (~$277m)
- Consulting: 23% (~$164m)
- Hosting: 13% (~$92m)
- BPO: 5% (~$36m). BPO services are provided on the Payer side
- Provider SaaS: 20% (~$142m).
Cognizant has higlighted the acquistion of TriZetto as an important step in the company's history:
- Towards a non-linear growth business. TriZetto is obiously an ISV business and has higher revenue per head (~$190k) than Cognizant (~$50k). Howevever, Cognizant is not buying a provider of plartforms: TriZetto is essentially a traditional ISV selling on premise perpetual licenses, where applications are implemented and customized by the client
- SaaS revenues represent 20% of revenues, BPO services 5% only - As a revenue generator with planned $1.5bn in additional revenues over 5 years. TriZetto has been a flat growth vendor overall in spite of M&As. In addition, the additional $1.5bn in additional revenues does not mean that Cognizant will triple revenues of TriZetto. Taking an assumption of revenue synergies happening towards the endof this 5-year period, TriZetto could reach sales of ~$1.3bn, up from $700m currenly. This is nice but hardly exponential for the company of the quality of Cognizant
- TriZetto with its software product business has high margins. Yet, TriZetto has lower operating margins than Cognizant. In addition, TriZetto under the ownershipby Apax Partners, offers little cost synergies. This means that under Cognizant, which will be focusing on revenue growth and investment in sales and products, the operating margin of TriZetto is likely to go down.
This lack of growth raises the question of price. Cognizant has not provided detailed information regarding its net profitability. Yet $2.7bn in cash for a company with flat revenues at best, a net profit likely to be in the $70m-$100m range and no cost synergies expected seems a bit expensive. However the market seems comfortable with the price Cognizant paid for TriZetto: Cognizant's share price was relatively flat after the annoucement.
This acquistion will put on hold any other significant M&A for Cognizant for while as the company will be focusing on small tuck-in acquistions to strengthen specific capabilities and focus on share buy-backs.
]]>On May 9, the Texas Health and Human Services Commission (HHSC) announced that the state was terminating its Medicaid claims administration contract with the Texas Medicaid and Healthcare Partnership (TMHP), a coalition of contractors led by Xerox. Cited for cause is that Xerox staff approved tens of thousands of prior-authorization (PA) requests for braces and other dental interventions for poor children that were not medically necessary. Texas Medicaid payments for orthodontic services grew from $6.5m in 2003 to $220.5m in 2010 (over 3,300%), while enrollment over the same period grew by just 33%.
The termination was followed by moves to agree a contract with Accenture (the largest TMHP subcontractor under Xerox) to assume TMHP's role in processing claims until a bidding process could determine a new lead vendor. The new contract has a three-year base period with two one-year extension options, with responsibility for processing over 12m claims per month. NelsonHall estimates the base-period contract value at just over $500m. Accenture has been involved as a subcontractor in the operation of the state's Medicaid claims payment system since 2004, when ACS started operations as prime contractor for fiscal agent services to the state.
In the re-bidding process, Texas is expected to divide the contracted work a few more ways across the vendor base to minimize the potential for disruption of Medicaid services, should additional conflicts surface in the future. Specifically, the state is targeting the following services: collection and analysis of managed-care transactions, staffing call centers and collecting drug-manufacturer rebates. All of these key services were previously provided by Xerox.
The damage to Xerox Services is substantial, in
- Revenues
- Its work to improve margins
- Reputation: more grist for competitors HP and CSC as they contest the MMIS system build at New York State (though the two activities are essentially different: one about the PA adjudication process, the other a new platform build)
]]>
Telecoms and media, Firstsource’s dominant sector (44% of revenues this quarter, around $56m), was the slowest growing vertical. The fastest growing was healthcare, with 15.8% y/y growth to ~$41m. This vertical was a contributor to the 17% growth in the U.S. Growth in the U.K. (15.3%) has been fuelled by the BFSI sector.
Attrition has decreased considerably in offshore centers in India and the Philippines (49.2% from 57.3% in Q2 FY 2014) and especially in onshore centers in the U.S. and Europe (33.8% from 47.4% in Q2 FY 2014); although these figures are still dramatically higher than its European and U.S. based peers. Attrition in its domestic serving centers continues to be a concern (92.8% from 85.6% in Q2 FY 2014).
Guidance for full FY 2014 remains upbeat:
- Moderate revenue growth fuelled by expansions from current customer management contracts, continued growth in the healthcare vertical and expected ramp up in BFSI collections
- Operating margin expansion of 150 to 200 bps, due to ongoing consolidations of low margin accounts, increasing efficiencies across business units, growth in offshore delivery and increasing collections business in Q4.